Understanding Vaginal Cancer
Vaginal cancer is a rare form of gynecologic cancer that develops in the tissue lining of the vagina. It accounts for only a small percentage of gynecologic cancers diagnosed each year and often begins as precancerous changes known as vaginal intraepithelial neoplasia (VaIN). Because symptoms can be subtle or absent in early stages, regular gynecologic exams and attention to any unusual bleeding or discharge are key to early detection.
At New York Gynecology Surgery & Endometriosis (NYGSE), our specialists provide advanced diagnosis and treatment for rare gynecologic cancers like vaginal cancer. We combine surgical precision, leading technology, and compassionate care to ensure every patient receives the best possible outcome and ongoing support through treatment and recovery.
COMMON QUESTIONS ABOUT vaginal Cancer
Cancer is a condition characterized by uncontrolled cell growth within the body. It is typically named after the specific area where it originates, even if it eventually spreads to other parts of the body.
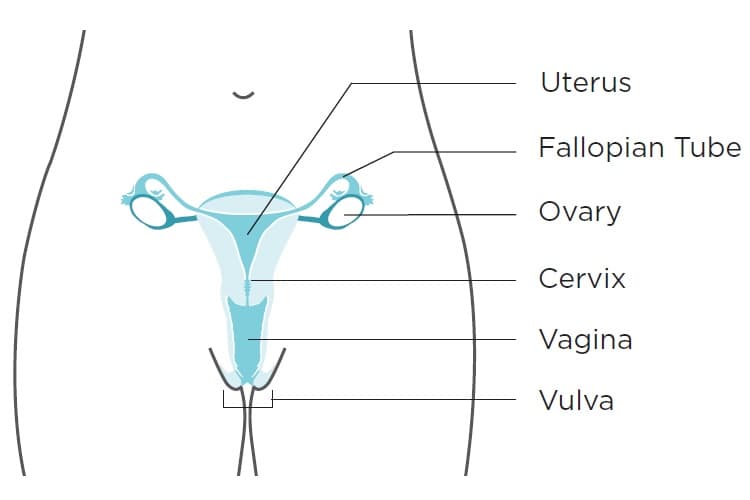
When cancer originates in the vagina, it is referred to as vaginal cancer. The vagina, also known as the birth canal, serves as the passage for menstrual blood and childbirth. It is connected to the cervix, the opening of the uterus, and surrounded by folds of skin known as the vulva.
Under normal circumstances, the vagina remains collapsed with its walls touching. However, during sexual intercourse and vaginal childbirth, the vaginal walls can expand due to numerous folds. The vaginal lining stays moist through mucus released from glands in the cervix.
The vaginal walls consist of a thin layer of cells known as the epithelium, containing squamous epithelial cells. Below the epithelium, the vaginal wall is composed of connective tissue, involuntary muscle tissue, lymph vessels, and nerves.
 Vaginal cancer is an extremely uncommon occurrence. While all women face some risk of these cancers, the likelihood of developing them is very low. Together, vaginal cancers account for approximately 7% of all gynecologic cancers diagnosed in the U.S.
Vaginal cancer is an extremely uncommon occurrence. While all women face some risk of these cancers, the likelihood of developing them is very low. Together, vaginal cancers account for approximately 7% of all gynecologic cancers diagnosed in the U.S.
Approximately 85% of vaginal cancer cases actually stem from cancer that has spread from other parts of the body, with about half of these originating from the cervix or uterus.
The vagina can be affected by five main types of cancer:
- Squamous cell carcinoma: This type of cancer originates in the cells lining the vagina, typically occurring near the cervix. Squamous cell carcinoma constitutes approximately 85% of vaginal cancer cases. Its development is gradual, often beginning with a precancerous condition known as vaginal intraepithelial neoplasia (VaIN), as described earlier.
- Adenocarcinoma: Adenocarcinoma starts in the glandular tissue of the vagina and accounts for about 5% to 10% of vaginal cancers.
- Clear cell adenocarcinoma: This particular cancer is associated with individuals whose mothers were exposed to the drug diethylstilbestrol (DES) during pregnancy between the late 1940s and 1971. It is a rare type of cancer, and it is estimated that approximately 1 in 1,000 people exposed to DES may develop vaginal cancer.
- Melanoma: While rare, melanoma can originate in the vagina. Melanomas typically occur on sun-exposed skin areas, but they can occasionally develop in regions with no sun exposure. They often present as dark-colored lesions with irregular borders.
- Sarcomas: These are uncommon tumors that can begin in the vagina. Several subtypes of sarcomas exist, each with its distinct characteristics.
Understanding the different types of vaginal cancer is crucial for early detection and appropriate treatment.
In the early stages, most vaginal cancers do not exhibit noticeable signs or symptoms. However, as the disease progresses, the following signs and symptoms may become apparent:
- Unusual vaginal discharge or abnormal bleeding: This bleeding may differ from your normal menstrual flow, either in terms of heaviness or timing. It could include bleeding after menopause, bleeding between periods, or any bleeding that is unusually prolonged or heavy for your typical pattern.
- Alterations in bathroom habits: You might experience blood in your stool or urine, find yourself using the bathroom more frequently than usual, or encounter constipation.
- Pelvic pain: Discomfort in the pelvic region, which refers to the area below your stomach and between your hip bones, may occur, particularly during urination or sexual intercourse.
As these symptoms can be indicative of vaginal cancer, it is essential to seek medical attention promptly if you experience any of these warning signs. Early detection and treatment can significantly improve the chances of successful outcomes.
Factors that may increase your risk of developing vaginal cancer include:
- Advancing age: As you reach the age of 60 or older, the risk of vaginal cancer tends to increase. The most common type, squamous cell carcinoma, is typically diagnosed around this age.
- Human papillomavirus (HPV) infection: Having HPV, a sexually transmitted virus, can elevate the risk of both cervical and vaginal cancer. Unprotected sexual activity with multiple partners and lack of HPV vaccination further heightens the likelihood of HPV infection.
- Vaginal intraepithelial neoplasia (VAIN): If you have VAIN, which involves abnormal cells in the vaginal lining (but not cancer cells), there is a potential for VAIN to progress to vaginal cancer. However, the reason why this progression occurs in some individuals and not others remains unclear. Having HPV increases the likelihood of developing VAIN.
- History of cervical cancer or cervical dysplasia: Women who have experienced cervical cancer or cervical dysplasia have a possibility of developing vaginal cancer in the future. The presence of abnormal cells in the cervix may contribute to the increased risk.
- Exposure to diethylstilbestrol (DES): DES, a synthetic estrogen prescribed between 1940 and 1971 to prevent pregnancy complications, can raise the risk of developing adenocarcinoma. If your birthing parent took DES during pregnancy, and you were exposed to it, your risk may be increased.
- Smoking: Smoking tobacco can double your risk of developing vaginal cancer.
It is essential to be aware of these risk factors and take necessary precautions, such as regular medical check-ups and lifestyle adjustments, to minimize the likelihood of developing vaginal cancer.
While it may not be possible to completely prevent vaginal cancer, there are measures you can take to reduce your risk:
Human papillomavirus (HPV) is a widespread virus consisting of over 200 different types, with more than 30 of them transmitted through close skin-to-skin contact during sexual activity. Most cases of cervical cancer and some instances of vaginal, vulvar, and other cancers are attributed to HPV infections.
The HPV vaccine is an effective way to safeguard against the types of HPV that commonly lead to cervical, vaginal, and vulvar cancers.
Here are the recommended guidelines for HPV vaccination:
- Preteens between the ages of 11 and 12 years should receive the HPV vaccine, with the option to start as early as age 9.
- The HPV vaccine is also recommended for individuals up to the age of 26 years, if they have not been vaccinated previously.
- For those older than 26 years, HPV vaccination is generally not advised. However, some adults aged 27 to 45 years, who have not been vaccinated before, may choose to consult their doctor about their risk of new HPV infections and the potential benefits of vaccination. It’s important to note that HPV vaccination in this age range may offer less protection, as many people might have already been exposed to HPV.
By following these vaccination recommendations and engaging in open discussions with healthcare professionals, you can take proactive steps to reduce the likelihood of HPV-related cancers, including vaginal cancer.
The recommended HPV vaccination schedule depends on the age at which it is initiated. If vaccination begins before reaching the age of 15, a two-dose schedule is advised, with the doses administered 6 to 12 months apart. However, for those who commence the vaccination series after their 15th birthday, a three-shot schedule is given.
It’s important to note that HPV vaccination serves as a preventive measure against new HPV infections, but it does not treat existing infections or diseases. Consequently, the HPV vaccine is most effective when administered before any exposure to HPV occurs. Even if you have received the HPV vaccine, regular screening for cervical cancer is essential to ensure early detection and appropriate management, as the vaccine does not provide protection against existing infections.
Screening for vaginal cancers in asymptomatic women is currently challenging as there is no simple and reliable test available for this purpose.
Screening involves using tests to detect a disease before any symptoms are evident. Effective cancer screening tests are instrumental in early disease detection, leading to more successful treatment outcomes. Diagnostic tests, on the other hand, are employed when a person exhibits symptoms. Their purpose is to identify the underlying cause of the symptoms. Diagnostic tests may also be conducted on individuals considered at high risk for cancer.
It is essential to recognize that the Pap test, although valuable for cervical cancer screening, does not screen for vaginal cancer. As no straightforward and dependable screening methods exist for most gynecologic cancers, except for cervical cancer, it becomes even more critical to be vigilant for potential warning signs and take measures to lower your risk.
Here are some proactive steps you can take:
- Be attentive to your body and be aware of what is normal for you.
- If you observe any changes in your body that are abnormal for you and could be indicative of vaginal or vulvar cancer, discuss them with your doctor and inquire about possible causes.
- Regularly visit your doctor for checkups. During these checkups, your doctor may perform a pelvic examination to identify signs of vaginal and vulvar cancer.
If a pelvic exam or Pap test raises concerns, your doctor may conduct a colposcopy. This procedure employs a lighted magnifying tool called a colposcope to examine your vagina and cervix for any unusual findings. A small tissue sample, known as a biopsy, might also be taken for further examination under a microscope by a specialist.
Upon diagnosing vaginal cancer, your doctor may order imaging tests and additional examinations to determine whether the cancer has spread to other parts of your body. This helps them establish the stage of the cancer and plan the appropriate treatment approach. Being proactive in monitoring your health and seeking timely medical attention can play a crucial role in detecting and managing vaginal cancer effectively.
Once a woman is diagnosed with vaginal cancer, medical professionals will conduct a process called staging to ascertain whether the cancer has spread and to what extent. Staging involves determining the amount of cancer present in the body, providing crucial information on the severity of the cancer and guiding the most appropriate treatment approach. Additionally, when discussing survival statistics, doctors use the cancer’s stage as a reference.
The stages of vaginal cancer are categorized from stage I (1) to IV (4). Generally, lower numbers indicate less cancer spread, while higher numbers, like stage IV, signify more extensive cancer spread. Although each individual’s experience with cancer is unique, cancers at similar stages tend to have comparable prognoses and are often treated using similar methods.
Both the FIGO (International Federation of Gynecology and Obstetrics) system and the AJCC (American Joint Committee on Cancer TNM staging system) are fundamentally similar when staging vaginal cancer.
They both utilize three key pieces of information to classify the cancer:
- The tumor’s extent (T): This entails assessing the size of the cancer and whether it has invaded the vaginal wall. Furthermore, the evaluation includes determining if the cancer has spread to nearby structures, such as the pelvic wall, which encompasses the internal cavity containing the female reproductive organs, rectum, bladder, and sections of the large intestine.
- The involvement of nearby lymph nodes (N): The staging process involves investigating whether the cancer has extended to the lymph nodes in the pelvic or groin (inguinal) area.
- The presence of distant metastasis (M): The staging evaluation includes determining whether the cancer has spread to distant lymph nodes or organs in the body.
By considering these three critical pieces of information, both staging systems provide a comprehensive assessment of the extent and progression of vaginal cancer, aiding in effective treatment planning and prognosis determination.
The T, N, and M staging components are further detailed by numbers or letters, offering more specific information about each factor. Higher numbers indicate a more advanced stage of cancer. After determining a person’s T, N, and M categories, this data is combined through a process known as stage grouping, resulting in an overall stage classification.
The table’s staging system primarily employs the clinical stage, which is determined based on the results of physical examinations, biopsies, and imaging tests conducted before any surgical procedures. Surgical staging, on the other hand, is established by examining the tissue removed during an operation. For further information on cancer staging, please refer to Cancer Staging.
The following system is the most recent AJCC system, which became effective in January 2018.
It’s important to note that these staging systems are not utilized for staging vaginal melanoma, as melanoma of the skin and vaginal melanoma are staged in a similar manner. For details on melanoma staging, refer to information about Melanoma Skin Cancer.
Given the complexity of vaginal cancer staging, it is advisable to ask your doctor to explain it to you in a manner that you can understand fully. This will ensure that you have a clear grasp of your specific situation and the implications of the staging process.
Stage 1 vaginal cancer indicates that the cancer has begun to grow into the vaginal wall but has not spread beyond that point.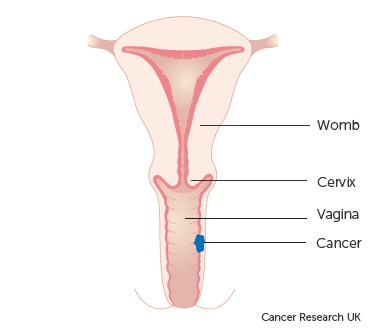
This stage is further divided into two groups:
- Stage 1A: The cancer is localized solely within the vagina and is not larger than 2cm in size. Additionally, it has not spread to nearby lymph nodes close to the vagina.
- Stage 1B: The cancer is confined to the vagina, but it measures more than 2cm in size. Similar to Stage 1A, it has not spread to lymph nodes in the vicinity of the vagina.
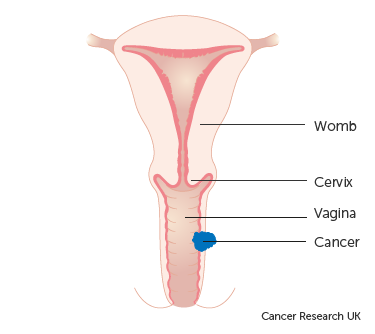
This stage is categorized into two groups:
- Stage 2A: In this stage, the cancer has extended beyond the confines of the vagina into the surrounding tissues. However, it has not reached the walls of the pelvis or nearby lymph nodes. Additionally, the size of the cancer is not larger than 2cm.
- Stage 2B: Similar to Stage 2A, the cancer has spread beyond the vagina into the surrounding tissues without reaching the walls of the pelvis or nearby lymph nodes. However, in this case, the size of the cancer is larger than 2cm.
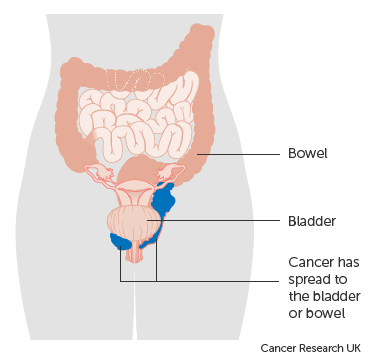
At this stage, the cancer has advanced beyond the vaginal area and infiltrated the side walls of the pelvis. Consequently, this can lead to urinary difficulties, such as experiencing pain or noticing blood during urination. Additionally, cancer cells might be detected in the lymph nodes located near the vagina.
This stage indicates advanced vaginal cancer, signifying that the cancer has metastasized to organs beyond the vagina.
Stage 4 is further divided into two groups:
- Stage 4A: In this group, the cancer has spread to other organs, such as the bladder or rectum (back passage).
Stage 4B represents an advanced condition where the cancer has extended to distant organs, such as the lungs or bones.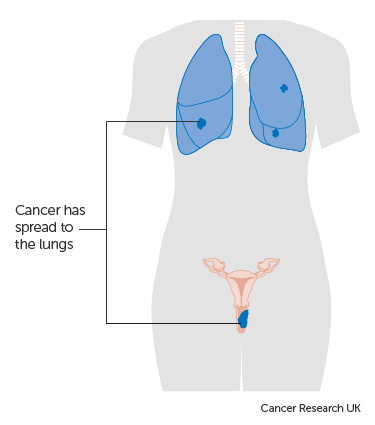
Patients diagnosed with vaginal cancer have access to various treatment options. These treatments can be categorized into standard procedures, which are the currently established therapies, and experimental approaches that are being investigated in clinical trials. Clinical trials are research studies conducted to enhance existing treatments or gather data on novel treatments for cancer patients. If clinical trials demonstrate that a new treatment is more effective than the standard one, it may replace the current standard of care.
Patients may consider participating in clinical trials to contribute to medical advancements. Some trials may only be available to patients who have not yet begun any treatment.
Surgery is one of the treatment options for vaginal cancer, and the following surgical procedures may be used:
- Wide local excision: This surgical procedure involves removing the cancer along with some surrounding healthy tissue.
- Vaginectomy: In this surgery, all or part of the vagina is removed. In some cases, skin grafts from other areas of the body may be necessary to reconstruct the vagina.
- Total hysterectomy: This surgery involves the removal of the uterus, including the cervix. Depending on the approach, it can be performed as a vaginal hysterectomy (via the vagina), a total abdominal hysterectomy (through a large incision in the abdomen), or a total laparoscopic hysterectomy (through a small incision in the abdomen using a laparoscope).
- Lymph node dissection: This surgical procedure entails removing lymph nodes, and a tissue sample is examined under a microscope to check for signs of cancer. It is also known as lymphadenectomy. If the cancer is in the upper vagina, pelvic lymph nodes may be removed, while lymph nodes in the groin may be removed if the cancer is in the lower vagina.
- Pelvic exenteration: This extensive surgery involves removing the lower colon, rectum, bladder, cervix, vagina, and ovaries. Nearby lymph nodes are also removed. As a result of this procedure, artificial openings (stoma) are created to allow urine and stool to be collected in external bags.
These surgical options are employed based on the specific characteristics of the vaginal cancer and the patient’s overall health condition. The choice of surgery will be determined in collaboration with the medical team to ensure the most appropriate and effective treatment plan.
Following the surgical removal of all visible cancer, certain patients may receive radiation therapy as a subsequent treatment to eliminate any remaining cancer cells. This post-surgery treatment, aimed at reducing the risk of cancer recurrence, is referred to as adjuvant therapy. Its purpose is to target any residual cancer cells that might not have been removed during the surgery, thereby enhancing the chances of long-term remission.
Radiation therapy
Radiation therapy is a cancer treatment that employs high-energy x-rays or other forms of radiation to either destroy cancer cells or prevent their further growth. There are two main types of radiation therapy:
- External radiation therapy involves utilizing a machine located outside the body to direct radiation towards the specific area of the body affected by cancer.
- Internal radiation therapy, also known as brachytherapy, entails using a sealed radioactive substance, such as needles, seeds, wires, or catheters, which are directly inserted into or placed near the cancer site to administer targeted radiation treatment.
The administration of radiation therapy is tailored to the specific type and stage of the cancer being treated. In the case of vaginal cancer, both external and internal radiation therapies are employed to target the disease effectively. Additionally, these radiation treatments can also serve as palliative therapy to alleviate symptoms and enhance the patient’s overall quality of life.
Chemotherapy is a cancer treatment that employs medications to halt the growth of cancer cells, either by inducing their death or preventing their division. The administration of chemotherapy can be through oral intake or injection into a vein or muscle, which allows the drugs to enter the bloodstream and reach cancer cells throughout the body (systemic chemotherapy). Alternatively, when chemotherapy is directly introduced into the cerebrospinal fluid, an organ, or a body cavity like the abdomen, its effects are primarily targeted at cancer cells in those specific areas (regional chemotherapy). The choice of chemotherapy method is determined based on the type and stage of the cancer being treated.
For squamous cell vaginal cancer, topical chemotherapy may be applied to the vagina using a cream or lotion, providing a localized treatment approach.
New types of treatment are being tested in clinical trials.
The following section provides an overview of treatments currently under investigation in clinical trials. Please note that not all new treatments being studied are mentioned in this summary.
Immunotherapy
Immunotherapy is a cancer treatment method that harnesses the patient’s own immune system to combat cancer. It involves using substances produced by the body or created in a laboratory to enhance, direct, or restore the body’s natural defenses against cancer. This approach is considered a form of biologic therapy.
Imiquimod, an immune response modifier, is currently being researched for its potential in treating vaginal lesions. It is applied to the skin in the form of a cream.
Radiosensitizers
Radiosensitizers are drugs that increase the sensitivity of tumor cells to radiation therapy. Combining radiation therapy with radiosensitizers has the potential to eliminate more tumor cells.
At NYGSE, we acknowledge that a cancer diagnosis can be a daunting and unsettling experience. That’s why we prioritize building teams centered around you. Our dedicated oncologists are here to support and assist you throughout this challenging journey, addressing any concerns or inquiries you may have. You can count on us to provide personalized care that meets your unique requirements and surpasses your expectations.
If you or a loved one are encountering symptoms that could be connected to cancer, we encourage you to contact us at your earliest convenience. We are here to help and offer the best possible care for your well-being.
Types of Gynecologic Cancer

Pankaj Singhal, MD, MS, MHCM
With over 12 years of experience in both academic and private healthcare, Dr. Singhal has trained more than 45 gynecologic surgeons and fellows in minimally invasive and oncologic procedures. He has pioneered new surgical techniques for endometriosis and laparoscopic surgery, completing more than 5,700 robotic-assisted cases nationwide. Renowned for taking on the most complex cases other centers turn away, Dr. Singhal continues to advance the standard of women’s surgical care.