Pelvic Organ Prolapse
Understanding Pelvic Organ Prolapse
Pelvic organ prolapse (POP) is a condition in which one or more of the pelvic organs, such as the uterus, bladder, or rectum, protrude or “fall” into the vagina due to weakened or damaged pelvic floor muscles and ligaments.
Pelvic organ prolapse can cause a variety of symptoms, including a feeling of heaviness or pressure in the pelvis, urinary incontinence or difficulty emptying the bladder, fecal incontinence or difficulty with bowel movements, pain or discomfort during sex, and vaginal bulging or protrusion.
There are different types of pelvic organ prolapse depending on which organ or organs are involved. Treatment for pelvic organ prolapse depends on the severity of the condition and the individual’s symptoms, but may include pelvic floor exercises, lifestyle changes, pessaries (devices inserted into the vagina to support the pelvic organs), or surgery.
Types of Pelvic Organ Prolapse
There are several types of pelvic organ prolapse, which are classified based on which organ or organs are involved:
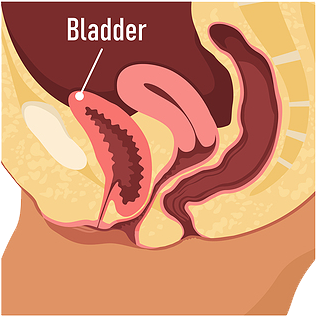
- Cystocele: This type of prolapse occurs when the bladder bulges into the front (anterior) vaginal wall.
- Rectocele: This type of prolapse occurs when the rectum bulges into the back (posterior) vaginal wall.
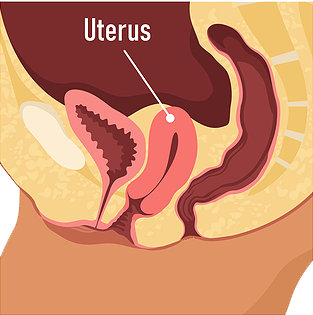
- Uterine prolapse: This type of prolapse occurs when the uterus falls into the vaginal canal.
- Vaginal vault prolapse: This type of prolapse occurs when the top of the vagina prolapses into the vaginal canal after the uterus has been removed.
- Enterocele: This type of prolapse occurs when a portion of the small intestine bulges into the vaginal canal.
- Pelvic floor dysfunction: This type of prolapse is a general term used to describe a weakness or dysfunction in the muscles, ligaments, and connective tissue that support the pelvic organs.
It’s worth noting that many women with pelvic organ prolapse have a combination of these types of prolapse. Treatment for pelvic organ prolapse will depend on the specific type and severity of the prolapse, as well as the individual’s symptoms and medical history.
Normal Anatomy
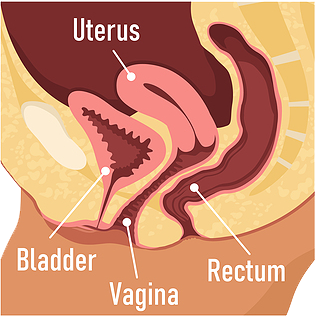
Cystocele
Uterine Prolapse
Rectocele
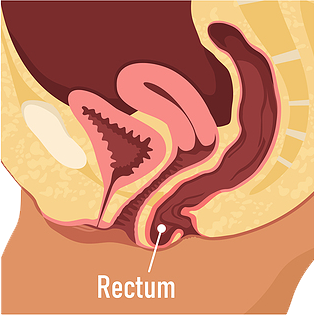
Image Source: Advanced Gynecology
What are the Symptoms of Pelvic Organ Prolapse?
Symptoms of pelvic organ prolapse can vary depending on the severity of the prolapse and which organs are affected, but some common symptoms include:
- A sensation of pressure or fullness in the pelvic region, as if something is falling out or dropping down
- A feeling of heaviness in the lower abdomen or pelvis
- Discomfort or pain during sexual intercourse
- Urinary problems, such as difficulty emptying the bladder completely, frequent urination, or urinary incontinence (leakage of urine)
- Bowel problems, such as constipation or fecal incontinence (leakage of stool)
- Lower back pain
- Vaginal bleeding or discharge
If you experience any of these symptoms, it is important to schedule an appointment with NYGS, who can help diagnose and treat pelvic organ prolapse.
How is Pelvic Organ Prolapse Diagnosed?
Pelvic organ prolapse (POP) is typically diagnosed through a combination of medical history, physical examination, and additional testing as needed.
During a physical examination, a healthcare provider may ask you to bear down (as if having a bowel movement) or cough, which can help reveal any bulging of the pelvic organs through the vaginal opening. They may also perform a pelvic exam to assess the degree of prolapse, check for any abnormalities or changes in the vaginal walls or cervix, and evaluate the strength of the pelvic floor muscles.
Additional testing may include:
- Imaging tests, such as a pelvic ultrasound or MRI, which can help visualize the prolapsed organs and any associated abnormalities or damage.
- Urodynamic testing, which assesses how well the bladder and urethra are functioning and can help diagnose any associated urinary problems.
- Colposcopy, which involves using a special instrument to examine the cervix and vaginal walls in more detail.
It is important to note that pelvic organ prolapse can often be diagnosed through a physical examination alone, and additional testing is only necessary if there are concerns about other potential underlying conditions or associated symptoms. It is always best to consult with a healthcare provider if you are experiencing symptoms or concerns about pelvic organ prolapse.
What is Prolapse Repair Procedure?
Prolapse repair procedure refers to the surgical procedures used to correct pelvic organ prolapse (POP), which is the condition in which one or more of the pelvic organs (such as the bladder, uterus, or rectum) bulge or descend into the vaginal wall or outside the body.
The specific prolapse repair procedure recommended will depend on the severity and type of prolapse, as well as the individual’s medical history and other factors. Common procedures include:
- Vaginal mesh surgery: In this procedure, a synthetic mesh is used to support the prolapsed organ and hold it in place. This surgery may be recommended for severe cases of POP or for women who have experienced a recurrence of POP after previous surgery.
- Sacrocolpopexy: This procedure involves using a mesh to attach the prolapsed organ to the sacrum (lower spine), providing support and preventing further descent.
- Hysterectomy: In some cases, a hysterectomy (surgical removal of the uterus) may be recommended as a treatment for POP, particularly if the prolapse involves the uterus.
- Colporrhaphy: This procedure involves repairing the vaginal wall and supporting tissues to correct the prolapse. In some cases, additional materials such as a synthetic mesh or the patient’s own tissue may be used to reinforce the repair.
It is important to note that prolapse repair procedures are generally considered safe and effective, but all surgical procedures carry some risk.
How Much is the Treatment of Pelvic Organ Prolapse ?
The cost of treatment for pelvic organ prolapse in the United States can vary widely depending on several factors such as the severity of the condition, the type of treatment needed, the location, and the healthcare provider.
- For mild cases, conservative treatments such as pelvic floor exercises or pessaries may be recommended. The cost of pessaries ranges from $50-$500, and pelvic floor therapy can cost between $150-$350 per session.
- For moderate to severe cases, surgical intervention may be required. The cost of surgery for pelvic organ prolapse can range from $5,000-$20,000 or more, depending on the type of surgery, the length of hospital stay, and other factors. The cost of surgical treatment also includes pre-operative and post-operative care, diagnostic tests, and any medications or medical supplies required.
- According to a 2021 report by the Healthcare Bluebook, the fair price range for laparoscopic pelvic organ prolapse repair surgery in the United States is between $11,958 and $27,427. This estimate includes the cost of the surgery, anesthesia, and facility fees, but does not include pre- or post-operative care or any additional charges that may be incurred.
It is important to note that health insurance may cover some or all of the cost of treatment, depending on the individual policy and the specific treatment recommended. It is always a good idea to check with your insurance provider to understand your coverage and potential out-of-pocket costs.
Pankaj Singhal, MD, MS, MHCM
- Industry expertise with over 12 years of experience in both academic & private health care settings, physician practice management and executive leadership.
- Trained over 45 gynecologic surgeons along with training fellows in minimally invasive gynecologic surgery and gynecology oncology, and has developed cutting edge, new surgical techniques for endometriosis and laparoscopic surgeries.
- One of the very few surgeons who have completed over 5,718 robot-assisted gynecologic surgeries in the entire United States.
- Known for taking on the most challenging surgery cases that other doctors/centers turn away.

Hear From Our Clients

Joetta Simonette
On May 3, 2018 at Good Samarital Hospital, due to cancer, you performed ovarian surgery on me.
It is now 5 years since that date – 5 years of wellness that has been accomplished through the grace of God guiding your hands and the support of your team and my loving family.
You are an excellent, compassionate and caring doctor who was confident of a good outcome, and so it is!
Thank you, thank you for these past wonderful years. May God continue to bless you. You are in my prayers!

RG Petkos
Power couple Dr. Singhal & Dr. Mclean are amazing!! My experience with them has been absolutely wonderful. I highly recommend either of them for so many reasons mainly for helping me get back some quality of life with my successful full hysterectomy being better than I expected.
The process from the beginning with them was a pleasure and I had quite a challenge beforehand so I’m very grateful that quality, professional, caring doctors still exist!!
I especially appreciate their proactive approach and feel the combination of the care and expertise they provide make for successful outcomes!!

Kimberly Quinde
Dr. Singhal was the doctor who took care of my mother Ivonne Guevara. My mother had gone to 2 other doctors who refused to take care of her fibroid. She was in pain for years and her fibroid had grown really big without her knowing. When my mom went to Dr Singhal she was met with calmness and reassurance that everything will be ok and he would help her get better. Dr. Singhal was so kind and caring all throughout the process.
He took all her worries away and my mom highly recommends him. She hopes every doctor can be as great as Dr. Singhal.
Everyone in his office was so nice to my mom and it was a great experience given the circumstances.
Frequently Asked Questions
Get answers to the most frequently asked questions about Pelvic Organ Prolapse.
Pelvic organ prolapse (POP) is a common condition and can range in severity from mild to severe. While it may not always be a serious condition, it can be uncomfortable and cause significant disruption to daily activities and quality of life.
In some cases, POP can lead to complications such as urinary incontinence, urinary tract infections, or difficulty with bowel movements. Severe cases of POP can also lead to sexual dysfunction and may require surgery to correct.
It is important to seek medical attention if you are experiencing symptoms of POP, such as a sensation of pressure or fullness in the pelvic region, discomfort or pain during sexual intercourse, or urinary or bowel problems.
Pelvic organ prolapse (POP) is a relatively common condition, particularly among women. The prevalence of POP increases with age and is estimated to affect up to 50% of women over the age of 50.
However, the actual incidence of POP may be higher than reported, as many women may not seek medical attention or report symptoms due to embarrassment or stigma surrounding pelvic floor disorders.
Several factors can contribute to the development of POP, including vaginal childbirth, aging, menopause, obesity, chronic constipation, and chronic coughing or straining. Women who have undergone hysterectomy or pelvic surgery may also be at increased risk.
While POP can be uncomfortable and disruptive to daily activities, it is treatable, and there are several conservative and surgical options available to manage symptoms and improve quality of life.
The recovery time for prolapse repair procedures can vary depending on the specific procedure, the extent of the repair, and the individual’s overall health and healing ability. In general, however, most women can expect to need several weeks to several months to fully recover from a prolapse repair procedure.
Immediately following the surgery, women may experience some pain, discomfort, and vaginal bleeding or discharge. They may also need to use a catheter to empty the bladder for a few days after surgery.
During the first few weeks after surgery, it is important to avoid heavy lifting, strenuous physical activity, and sexual intercourse. Women may also need to avoid standing or sitting for extended periods of time, and may need to use a stool softener to prevent constipation.
Over time, women can gradually increase their activity level and return to normal daily activities, but it may take several weeks to several months to fully recover and regain strength and stamina.
It is important to follow all post-operative instructions provided by the healthcare provider and attend any recommended follow-up appointments to ensure proper healing and monitor for any complications.
There are several ways to relieve symptoms of pelvic prolapse, including:
- Pelvic floor muscle exercises: Kegel exercises and other pelvic floor exercises can help strengthen the muscles that support the pelvic organs and improve symptoms of prolapse.
- Pessary: A pessary is a medical device that is inserted into the vagina to support the pelvic organs and alleviate symptoms of prolapse.
- Lifestyle changes: Maintaining a healthy weight, avoiding heavy lifting, and quitting smoking can help relieve symptoms of prolapse.
- Physical therapy: Working with a physical therapist who specializes in pelvic floor health can help improve symptoms of prolapse through exercises and other therapies.
- Estrogen therapy: In some cases, estrogen therapy may be recommended to help improve vaginal tissue health and alleviate symptoms of prolapse.
- Surgery: In more severe cases of prolapse, surgery may be recommended to correct the prolapse and relieve symptoms.
Kegel exercises are a type of pelvic floor muscle exercise that involves contracting and relaxing the muscles that support the pelvic organs (such as the bladder, uterus, and rectum). These exercises are designed to help strengthen the pelvic floor muscles, which can help improve symptoms of pelvic organ prolapse, urinary incontinence, and other conditions that affect the pelvic region.
To perform Kegel exercises, it is important to first identify the correct muscles to target. This can be done by trying to stop the flow of urine during urination – the muscles used to stop the urine flow are the same muscles used in Kegel exercises.
Once the correct muscles are identified, Kegel exercises can be performed by:
- Contracting the pelvic floor muscles by squeezing them for 3-5 seconds
- Relaxing the muscles for 3-5 seconds
- Repeating the exercise for a total of 10 repetitions, 3-4 times per day
Over time, women can gradually increase the duration and intensity of the contractions, aiming to hold the muscles contracted for up to 10 seconds at a time. Kegel exercises can be performed anywhere and at any time, making them a convenient and easy way to improve pelvic floor muscle strength.
A pessary is a medical device that is inserted into the vagina to support the pelvic organs and alleviate symptoms of pelvic organ prolapse (POP). Pessaries are typically made of silicone or rubber and come in a variety of shapes and sizes to accommodate different women’s anatomy and levels of prolapse.
The pessary works by supporting the pelvic organs and helping to keep them in their proper position. This can help alleviate symptoms such as pelvic pressure, discomfort, and urinary incontinence.
Pessaries are typically prescribed by a healthcare provider and are fitted specifically to each individual’s anatomy. They may need to be adjusted or replaced over time to ensure proper fit and function.
While pessaries can be an effective non-surgical treatment option for POP, they do require regular cleaning and maintenance to prevent infection and other complications. Women who use a pessary should also be monitored regularly by their healthcare provider to ensure that it is functioning properly and to check for any signs of complications.
Yes, surgery can be an effective treatment option for correcting pelvic support problems, such as pelvic organ prolapse (POP). The specific surgical approach used will depend on the severity and underlying causes of the prolapse, as well as the individual’s medical history and preferences.
There are several types of surgical procedures that can be used to correct pelvic support problems. These may include:
- Vaginal wall repair: This procedure involves repairing the stretched or weakened tissue in the vaginal wall to restore support to the pelvic organs.
- Hysterectomy: This surgical procedure involves removing the uterus, which can help alleviate symptoms of prolapse in women with uterine prolapse.
- Sacrocolpopexy: This procedure involves using mesh or other materials to provide support to the prolapsed organs by attaching them to the sacrum (the triangular bone at the base of the spine).
- Colpocleisis: This procedure involves closing off the vaginal canal, effectively removing the prolapsed organs and creating a barrier to prevent further prolapse.
Surgery for pelvic support problems can be very effective in improving symptoms and restoring normal function to the pelvic region. However, like any surgery, it does carry some risks and potential complications. Women considering surgery for pelvic support problems should discuss the benefits and risks of the procedure with their healthcare provider and make an informed decision based on their individual case and medical history.
Whether or not your insurance will cover prolapse repair procedure depends on your individual insurance plan and the specific procedure recommended by your healthcare provider.
In general, most insurance plans will cover medically necessary surgical procedures, including those used to treat pelvic organ prolapse. However, coverage can vary depending on the specific procedure, the reason for the surgery, and the terms of the insurance policy.
It is important to check with your insurance provider to determine the specifics of your coverage, including any deductibles, co-pays, or out-of-pocket expenses you may be responsible for.
In some cases, insurance may not cover certain procedures or may require pre-authorization before the surgery can be scheduled. Your healthcare provider or their staff can help you navigate the insurance process and work with your insurance provider to obtain the necessary coverage for your treatment.
Hospital Affiliations


Request an Appointment
"*" indicates required fields
