Vulvar Cancer
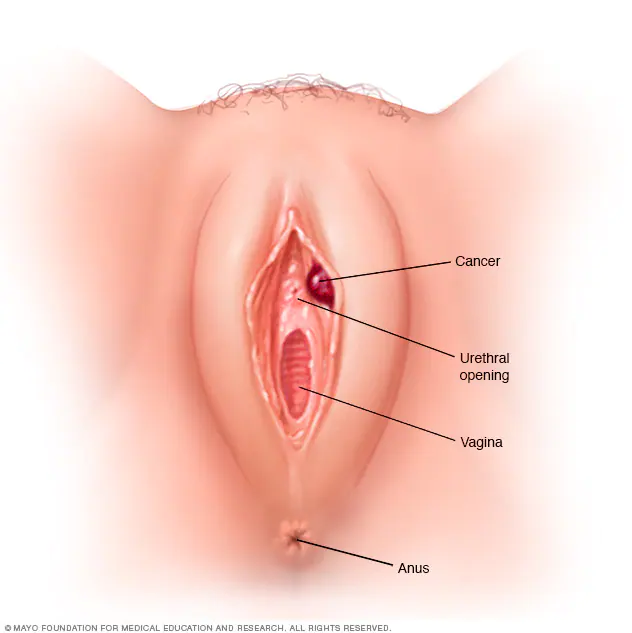
What is Vulvar Cancer?
Vulvar cancer is a form of cancer that develops on the external surface of the female genitalia. The vulva refers to the skin area encircling the urethra and vagina, which includes:
- The lips encompassing the vagina (labia minora and labia majora).
- The clitoris, a sexual organ vital in achieving sexual climax.
- The Bartholin’s glands, two small glands on each side of the vagina.
Typically, vulvar cancer manifests as a lump or sore on the vulva, often accompanied by itching. While it can occur at any age, it is more commonly diagnosed in older adults.
The treatment for vulvar cancer generally involves surgical intervention to remove the cancerous tissue along with a small portion of the surrounding healthy tissue. In some cases, extensive surgery may be necessary, which could involve the removal of the entire vulva. The prognosis and complexity of the surgery tend to improve significantly when vulvar cancer is detected at an early stage.
In the United States, approximately 6,000 new cases of vulvar cancer are reported each year. Among these cases, roughly half are attributed to human papillomavirus (HPV), and the other half are associated with lichen sclerosus. Vulvar cancer is considered a highly uncommon form of cancer, making up only 0.6 percent of all cancer diagnoses in women.
Types of Vulvar Cancer
Vulvar cancer encompasses various types, with squamous cell carcinoma being the most prevalent. Approximately 90% of vulvar cancers are squamous cell carcinomas, mainly found on the labia.
Squamous cell carcinoma can develop from a precancerous condition known as vulva intraepithelial neoplasia (VIN). VIN involves cell changes that may or may not progress to cancer. It is crucial to note that VIN is considered a premalignant growth, meaning it is not yet cancerous. VIN is further categorized into two groups based on cellular appearance under a microscope: “usual-type VIN” typically seen in younger women, associated with human papillomavirus (HPV), and “differentiated VIN,” less common and prevalent in older women, not linked to HPV. Differentiated VIN often occurs in women with lichen sclerosus, a skin condition that is likely to be diagnosed by a gynecologist and may or may not be known prior to VIN. It’s important to be aware that this form of VIN can potentially develop into a fast-moving, aggressive squamous cancer. Refer to Risk Factors and Prevention for more information on HPV, precancerous vulvar conditions, and lichen sclerosus.
Other less common types of vulvar cancer include:
- Verrucous carcinoma: This is a slow-growing subtype of squamous cell carcinoma that has a wart-like appearance.
- Adenocarcinoma: Originating in the Bartholin’s glands or vulvar sweat glands, adenocarcinoma constitutes a small percentage of vulvar cancers. It is typically found on the sides of the vaginal opening.
- Melanoma: Accounting for about 2% to 4% of vulvar cancers, melanoma is a type of skin cancer usually found in sun-exposed areas of the body but can occasionally develop in non-sun-exposed regions. When it occurs in the vulva, it is most frequently found on the clitoris or labia minora. Women with melanoma elsewhere on their body face an increased risk of vulvar melanoma. Treatment for vulvar melanoma often follows approaches similar to those used for melanoma in other parts of the body.
- Sarcoma: Sarcoma involves tumors in the connective tissue beneath the skin.
It is essential to recognize these different types of vulvar cancer as they may necessitate distinct treatment strategies based on their specific characteristics.
Symptoms of Vulvar Cancer
The indications and symptoms of vulvar cancer can encompass the following:
- Persistent itch in the vulva
- Pain, soreness, or tenderness in the vulva
- Raised and thickened patches of skin that may appear red, white, or dark
- Presence of a lump or wart-like growth on the vulva
- Bleeding from the vulva or blood-stained vaginal discharge between periods
- Development of an open sore in the vulva
- Experiencing a burning pain during urination
- Noticeable changes in shape or color of a mole on the vulva
If any of these signs or symptoms persist or cause concern, it is essential to seek medical evaluation promptly for a thorough assessment and appropriate management.
Causes of Vulvar Cancer
The development of vulvar cancer cannot be predicted with certainty. While some women may experience these cancers without apparent high risk factors, certain elements may increase the likelihood of developing vaginal or vulvar cancer. These factors include:
- Increasing Age: The risk of vulvar cancer rises with age, with the average age at diagnosis being around 65 years.
- Exposure to Human Papillomavirus (HPV): HPV, a sexually transmitted infection, elevates the risk of various cancers, including vulvar and cervical cancers. Many sexually active individuals, especially the young, may come into contact with HPV, but in most cases, the infection clears up on its own. However, for some, it can cause cellular changes that increase the risk of cancer in the future.
- Smoking: For women with an HPV infection, smoking may hinder the body’s immune system from effectively clearing the HPV infection.
- Weakened Immune System: Individuals who take immune-suppressing medications (e.g., organ transplant recipients) or have conditions that weaken the immune system (e.g., human immunodeficiency virus, HIV) are at an increased risk of vulvar cancer.
- History of Precancerous Conditions of the Vulva: Vulvar intraepithelial neoplasia, a precancerous condition, raises the risk of vulvar cancer. Although most cases of vulvar intraepithelial neoplasia do not progress to cancer, a small number may develop into invasive vulvar cancer. As a precaution, doctors may recommend treatment to remove the abnormal cell area and conduct regular follow-up checks.
- Skin Condition Involving the Vulva: Lichen sclerosus is a condition that affects the vulvar skin, causing it to become thin and itchy, thereby increasing the risk of vulvar cancer.
Though these factors can contribute to an increased risk, it’s important to remember that not everyone with these risk factors will develop vulvar cancer, and some cases may occur without any identifiable risk factors. Regular check-ups and early detection remain essential for timely management and improved outcomes.
Lower Your Chance of Getting Vulvar Cancer
Various factors contribute to different types of cancer, including vulvar cancer. Researchers are actively investigating the causes of vulvar cancer and exploring preventive measures. While there is no guaranteed method to completely prevent vulvar cancer, certain steps can be taken to potentially reduce the risk. It is crucial to discuss your individual risk of cancer with your healthcare team for personalized information.
To aid in the detection of vulvar cancer, the doctor will review your family medical history, conduct a comprehensive physical examination, and perform a gynecologic exam focusing on the pelvis. During this exam, the doctor will carefully assess the vulva and perform checks on the uterus, vagina, cervix, and other reproductive organs for any unusual changes. Regular pelvic examinations are valuable in identifying cancer or precancerous conditions at an early stage.
Moreover, research has revealed specific factors that can potentially help in preventing vulvar cancer:
- Delaying first sexual intercourse until the late teens or older.
- Avoiding sexual intercourse with multiple partners.
- Avoiding sexual intercourse with individuals who have had numerous partners.
- Practicing safe sex, including condom use. Nevertheless, it is essential to acknowledge that condoms cannot provide complete protection against HPV. Abstinence from sexual intercourse remains the only method for full protection against HPV.
- Undergoing regular gynecologic examinations to detect and treat precancerous conditions.
- Quitting tobacco use for individuals who smoke.
By adopting these preventive measures and staying vigilant with regular check-ups, you can take proactive steps toward reducing the risk of vulvar cancer and promoting overall health. Remember to consult with your healthcare provider for personalized guidance and recommendations.
Detection of Vulvar Cancer
The diagnostic process for vulvar cancer involves various tests and procedures, including:
- Physical examination of the vulva: Your doctor will perform a thorough physical examination of your vulva to identify any abnormalities or concerning signs.
- Colposcopy examination: During a colposcopy, a special magnifying device is utilized to closely inspect the vulva for any abnormal areas. This enables a more detailed assessment of any suspicious regions.
- Biopsy: If an area of the vulva appears suspicious, a biopsy may be recommended to determine whether it is cancerous. During the biopsy procedure, the area is numbed with a local anesthetic, and a scalpel or other specialized cutting tool is used to remove a sample of the suspicious tissue for further testing.
These tests and procedures play a crucial role in diagnosing vulvar cancer accurately. If you experience any symptoms or have concerns about your vulvar health, it is essential to seek prompt medical evaluation to ensure timely diagnosis and appropriate management.
Stages of Vulvar Cancer
Stage groupings in cancer are determined based on the values of T (Tumor), N (Nodes), and M (Metastasis). These groupings provide an overall description of the extent of cancer in the body.
T = Tumor: This refers to the location and size of the primary tumor.
N = Nodes: Indicates whether the tumor has spread to nearby lymph nodes.
M = Metastasis: Determines whether cancer has spread to other parts of the body.
Each letter is accompanied by five numbered stages, ranging from 0 to 4, depending on the extent of cancer spread. Lower stage numbers indicate that the cancer cells closely resemble normal cells, making them more manageable and potentially curable. Conversely, higher stage numbers signify a deeper spread of the cancer, which may require more complex treatments and have a more challenging prognosis. Understanding the stage grouping is critical for determining the appropriate treatment plan and predicting the course of the disease.
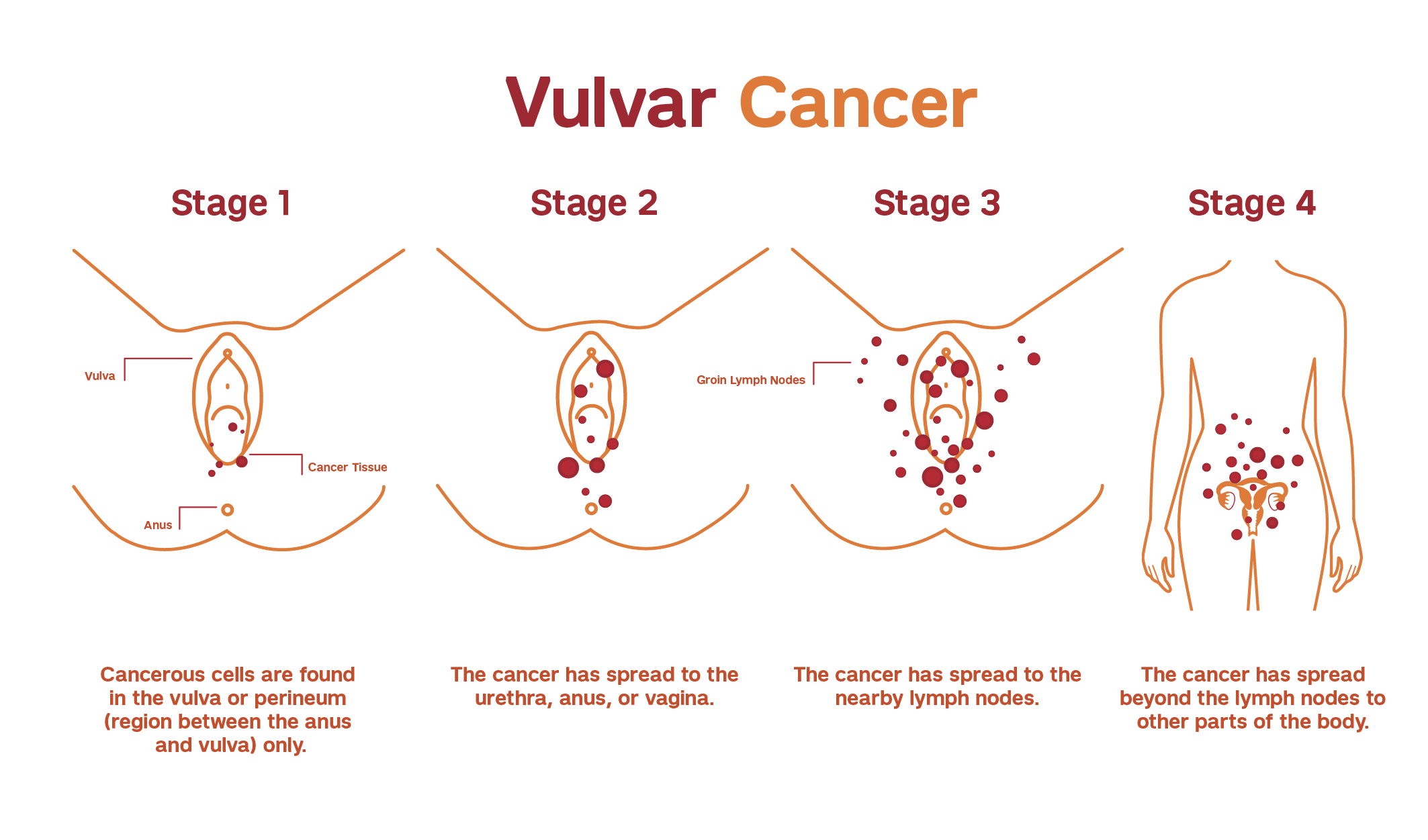
Stage groupings for invasive vulvar cancer are represented by Roman numerals, with values ranging from I (1) to IV (4). A higher stage number indicates a more advanced and extensive spread of the cancer.
The staging process for invasive vulvar cancer is determined by surgical findings and pathology. However, it’s important to note that stages for vulvar melanoma are distinct and not discussed in this context.
Stage I. The cancer is located either in the vulva or in the area between the opening of the rectum and the vagina (perineum), or it may involve both regions. At this stage, the cancer has not spread to nearby lymph nodes or other parts of the body. This stage is further divided into two substages:
Stage IA. The tumor size is limited to 2 centimeters (cm) or smaller, and its depth of growth into the vulvar tissue is no more than 1 millimeter (mm).
Stage IB. The tumor measures over 2 centimeters (cm) in size and/or has extended more than 1 millimeter (mm) beneath the surface of the vulvar skin.
- Stage II. The tumor can be of any size and has extended beyond the vulva, reaching nearby sites such as the urethra, lower vagina, or anus. However, it has not spread to lymph nodes or other distant parts of the body.
Stage III. The cancer is present in either the vulva, the perineum, or both. There is a possibility that it has spread to the urethra, lower vagina, or anus, but it has not extended to organs in distant parts of the body. This stage is further divided into three substages.:
Stage IIIA. The cancer has metastasized either to a single lymph node measuring at least 5 mm across, or to one or two lymph nodes that are less than 5 mm across.
Stage IIIB. The cancer has disseminated to three or more lymph nodes, each measuring no more than 5 mm across, or it has spread to two or more lymph nodes, each measuring more than 5 mm across.
Stage IIIC. The cancer has extended to adjacent lymph nodes, and in at least one of these nodes, the cancer is growing beyond its outer layer, a condition known as extracapsular spread.
Stage IV. This stage is divided into 2 substages:
The cancer is present in either the vulva, the perineum, or both. It is uncertain whether it has spread to the urethra, lower vagina, or anus. However, it has extended to nearby lymph nodes, which are adhering to deeper tissues or have developed ulcers.
The cancer has progressed beyond adjacent tissues and reached the upper part of the urethra, upper vagina, bladder, rectum, or pelvic bone. It is uncertain whether it has also spread to nearby lymph nodes.
Treatment of Vulvar Cancer
The treatment options for vulvar cancer are determined by factors such as the type, stage, and location of the cancer, as well as your overall health and personal preferences.
Surgery
Surgical procedures used to treat vulvar cancer include:
- Excision (Wide Local Excision or Radical Excision): The cancer and a small portion of surrounding healthy tissue are surgically removed to ensure complete elimination of cancerous cells.
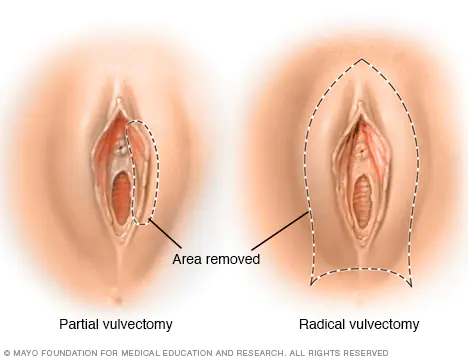
- Vulvectomy (Partial or Radical): For larger cancers, surgery may involve the removal of part of the vulva (partial vulvectomy) or the entire vulva, including underlying tissue (radical vulvectomy). In some cases, radiation therapy and chemotherapy may be used before surgery to shrink the tumor, potentially allowing for a less extensive operation.
- Sentinel Node Biopsy: To assess the presence of cancer in the lymph nodes, a procedure called sentinel node biopsy is performed. It identifies the lymph nodes most likely to contain cancer, which can then be removed and examined. If cancer is not detected in these lymph nodes, the likelihood of it being present in other lymph nodes is low.
- Removal of Multiple Lymph Nodes: If cancer has spread to the lymph nodes, a significant number of lymph nodes may be removed to reduce the risk of cancer spreading to distant areas of the body.
Undergoing surgery involves potential complications, including infection and challenges related to healing around the incision site. Additionally, when lymph nodes are removed, there is a risk of developing lymphedema, a condition characterized by fluid retention and swelling in the legs.
Radiation Therapy
Radiation therapy employs high-powered energy beams, such as X-rays and protons, to target and destroy cancer cells. In the context of vulvar cancer, radiation therapy is often delivered through a machine that moves around the body, precisely directing radiation to specific points on the skin (known as external beam radiation).
This treatment approach is sometimes used to reduce the size of large vulvar cancers, increasing the likelihood of a successful surgery. Combining radiation therapy with chemotherapy is also an option, as chemotherapy can render cancer cells more susceptible to the effects of radiation.
Furthermore, if cancer cells are detected in the lymph nodes, your doctor may recommend radiation therapy to the area surrounding the lymph nodes. This is intended to eliminate any remaining cancer cells after surgery. In certain cases, radiation therapy is combined with chemotherapy to maximize its effectiveness in these situations.
Chemotheraphy
Chemotherapy is a medical treatment that employs chemical substances to target and destroy cancer cells. Typically, these drugs are administered either through a vein in the arm or by mouth.
In cases of advanced vulvar cancer that has spread to distant areas of the body, chemotherapy may be considered as a treatment option.
Combining chemotherapy with radiation therapy is also utilized to reduce the size of large vulvar cancers, enhancing the chances of a successful surgical procedure. Additionally, when cancer has spread to the lymph nodes, combining chemotherapy with radiation therapy can be an effective approach in treatment.
Targeted Drug Theraphy
Targeted drug treatments are designed to specifically target and inhibit the abnormalities found within cancer cells. By blocking these specific abnormalities, targeted drug treatments can trigger the death of cancer cells.
For individuals with advanced vulvar cancer, targeted therapy may be considered as a potential treatment option.
Immunotherapy
Immunotherapy harnesses the power of your immune system to combat cancer. In some cases, cancer cells can evade detection by producing proteins that enable them to evade the immune system’s attack. Immunotherapy intervenes in this process, allowing the immune system to recognize and target cancer cells effectively.
For individuals with advanced vulvar cancer, immunotherapy could be considered as a potential treatment option.
NYGS Approach
We recognize that receiving a cancer diagnosis can be an overwhelming and daunting experience. At NYGS, our dedicated teams are centered around your well-being. Our skilled oncologists are committed to supporting you through this challenging journey, offering guidance and addressing any concerns you may have.
Rest assured that we are here for you, and our utmost priority is to cater to your individual needs, striving to surpass your expectations. If you or a loved one are experiencing symptoms that could be related to cancer, we urge you to contact us as soon as possible. Your health and care are of the utmost importance to us.
Pankaj Singhal, MD, MS, MHCM
- Industry expertise with over 12 years of experience in both academic & private health care settings, physician practice management and executive leadership.
- Trained over 45 gynecologic surgeons along with training fellows in minimally invasive gynecologic surgery and gynecology oncology, and has developed cutting edge, new surgical techniques for endometriosis and laparoscopic surgeries.
- One of the very few surgeons who have completed over 5,718 robot-assisted gynecologic surgeries in the entire United States.
- Known for taking on the most challenging surgery cases that other doctors/centers turn away.

Hear From Our Clients

Joetta Simonette
On May 3, 2018 at Good Samarital Hospital, due to cancer, you performed ovarian surgery on me.
It is now 5 years since that date – 5 years of wellness that has been accomplished through the grace of God guiding your hands and the support of your team and my loving family.
You are an excellent, compassionate and caring doctor who was confident of a good outcome, and so it is!
Thank you, thank you for these past wonderful years. May God continue to bless you. You are in my prayers!

RG Petkos
Power couple Dr. Singhal & Dr. Mclean are amazing!! My experience with them has been absolutely wonderful. I highly recommend either of them for so many reasons mainly for helping me get back some quality of life with my successful full hysterectomy being better than I expected.
The process from the beginning with them was a pleasure and I had quite a challenge beforehand so I’m very grateful that quality, professional, caring doctors still exist!!
I especially appreciate their proactive approach and feel the combination of the care and expertise they provide make for successful outcomes!!

Kimberly Quinde
Dr. Singhal was the doctor who took care of my mother Ivonne Guevara. My mother had gone to 2 other doctors who refused to take care of her fibroid. She was in pain for years and her fibroid had grown really big without her knowing. When my mom went to Dr Singhal she was met with calmness and reassurance that everything will be ok and he would help her get better. Dr. Singhal was so kind and caring all throughout the process.
He took all her worries away and my mom highly recommends him. She hopes every doctor can be as great as Dr. Singhal.
Everyone in his office was so nice to my mom and it was a great experience given the circumstances.
Hospital Affiliations


Request an Appointment
"*" indicates required fields