Cervical Cancer
What is Cervical Cancer?
Cancer is a condition characterized by the abnormal growth and multiplication of cells in the body. The name of the cancer is usually derived from the body part where it originates, regardless of whether it later spreads to other areas of the body. In the case of cancer starting in the cervix, it is referred to as cervical cancer. The cervix is the connecting passage between the vagina (birth canal) and the upper part of the uterus, which is where a fetus develops during pregnancy.
All women, irrespective of their age, are susceptible to cervical cancer, though it occurs more frequently in women aged 30 and above. Cervical cancer is primarily caused by a prolonged infection with specific types of human papillomavirus (HPV), a common virus transmitted during sexual activity. Although roughly half of sexually active individuals acquire HPV at some point in their lives, few women develop cervical cancer.
Regular screening tests and HPV vaccination can aid in preventing cervical cancer. If detected early, cervical cancer is highly curable and linked with extended survival and a good quality of life.
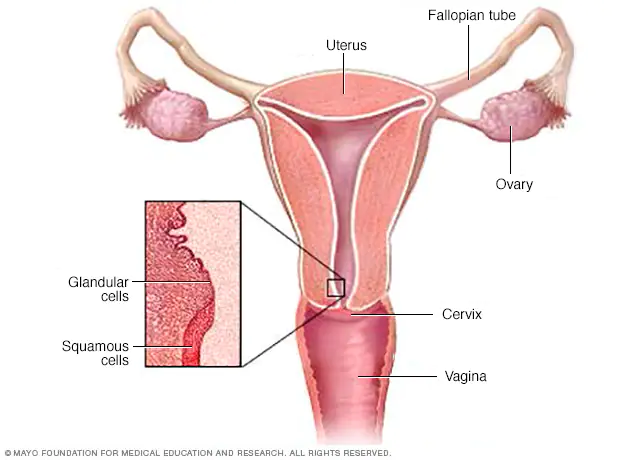
The cervix is the lower, narrow part of the uterus that connects the uterus to the vagina. It is composed of several different parts, including:
- External os: This is the opening of the cervix that faces downward into the vagina.
- Internal os: This is the opening of the cervix that faces upward into the uterus.
- Endocervical canal: This is the passage that runs through the center of the cervix and connects the internal and external os.
- Transformation zone: This is the area of the cervix where the squamous epithelial cells (from the vagina) and columnar epithelial cells (from the uterus) meet. This area is most prone to developing precancerous and cancerous changes.
- Cervical stroma: This is the connective tissue that makes up the bulk of the cervix and contains blood vessels, lymphatic vessels, and nerves.
Understanding the different parts of the cervix is important for screening and diagnosing cervical cancer, as well as for planning treatment.
Types of Cervical Cancer
There are several types of cervical cancer, which are classified based on the type of cell where the cancer originates. The two most common types of cervical cancer are:
- Squamous cell carcinoma: This type of cancer begins in the thin, flat cells that line the outer part of the cervix. Squamous cell carcinoma accounts for about 80-90% of all cervical cancers.
- Adenocarcinoma: This type of cancer starts in the glandular cells that line the inside of the cervix. Adenocarcinoma accounts for about 10-20% of all cervical cancers.
There are also some less common types of cervical cancer, including:
- Adenosquamous carcinoma: This is a type of cancer that has features of both squamous cell carcinoma and adenocarcinoma.
- Small cell carcinoma: This is a rare and aggressive type of cervical cancer that begins in the nerve cells.
- Neuroendocrine tumors: These are rare tumors that develop from the hormone-producing cells in the cervix.
- Glassy cell carcinoma: This is an extremely rare and aggressive form of cervical cancer.
Understanding the type of cervical cancer a patient has is essential for determining the best course of treatment. Treatment options will depend on the type and stage of cancer, as well as the patient’s overall health and preferences.
Symptoms of Cervical Cancer
In its early stages, cervical cancer often does not cause any noticeable symptoms. However, as the cancer grows and spreads, it can cause a range of symptoms, which may include:
- Abnormal vaginal bleeding: This may include bleeding between periods, after sex, or after menopause.
- Unusual vaginal discharge: This may be watery, thick, or have a foul odor.
- Pain during sex: This may be due to the tumor pressing against the cervix or surrounding tissues.
- Pelvic pain: This may occur in the lower abdomen or back.
- Painful urination: This may be a sign that the tumor has spread to nearby tissues.
- Swelling in one or both legs: This may occur if the cancer has spread to the lymph nodes or other organs.
It is important to note that many of these symptoms can be caused by conditions other than cervical cancer. However, if any of these symptoms persist for more than a few weeks, it is important to see a healthcare provider for an evaluation. Regular cervical cancer screening tests, such as Pap tests and HPV tests, can also help detect the cancer in its early stages, before it causes symptoms.
Causes of Cervical Cancer
The main cause of cervical cancer is a long-term infection with certain types of the human papillomavirus (HPV). HPV is a common sexually transmitted virus, and most sexually active people will be infected with HPV at some point in their lives. However, in most cases, the body’s immune system will clear the virus without any problems.
In some cases, however, the virus can cause changes in the cells of the cervix, which can lead to cervical cancer over time. Other factors that may increase the risk of cervical cancer include:
- Smoking: Women who smoke are more likely to develop cervical cancer than non-smokers.
- Weakened immune system: Women with weakened immune systems, such as those who have HIV/AIDS or who have had an organ transplant, are at increased risk of cervical cancer.
- Family history: Women with a family history of cervical cancer may be at increased risk.
- Long-term use of birth control pills: Women who have used birth control pills for several years may have a slightly increased risk of cervical cancer.
- Multiple sexual partners: Women who have had multiple sexual partners may be at increased risk of cervical cancer, as they are more likely to be exposed to HPV.
- Having sex at an early age: Women who had sex for the first time at a young age may be at increased risk of cervical cancer.
It is important to note that having one or more of these risk factors does not mean that a woman will definitely develop cervical cancer. However, women with one or more risk factors may benefit from more frequent cervical cancer screening or other preventive measures.
Lower Your Chance of Getting Cervical Cancer
There are several steps women can take to lower their chances of getting cervical cancer:
- Get vaccinated: The HPV vaccine can protect against the types of HPV that are most likely to cause cervical cancer. The vaccine is recommended for girls and boys between the ages of 9 and 26.
- Practice safe sex: Using condoms during sex can help reduce the risk of HPV infection.
- Get regular cervical cancer screenings: Women should start getting regular Pap tests at age 21, or earlier if they are sexually active before age 21. Women over age 30 may also consider getting an HPV test along with their Pap test. These tests can help detect any abnormal cells in the cervix before they become cancerous.
- Quit smoking: Women who smoke are more likely to develop cervical cancer than non-smokers. Quitting smoking can help reduce this risk.
- Maintain a healthy diet and exercise regularly: A healthy lifestyle can help support the immune system and reduce the risk of many types of cancer, including cervical cancer.
- Limit the number of sexual partners: Women who have had multiple sexual partners are at increased risk of HPV infection and cervical cancer.
- Practice good hygiene: Women should avoid using douches or other feminine hygiene products, which can disrupt the natural balance of bacteria in the vagina and increase the risk of infection.
By following these steps, women can lower their risk of developing cervical cancer and improve their overall health.
Detection of Cervical Cancer
There are two main tests used to detect cervical cancer:
- Pap test: During a Pap test, a healthcare provider collects cells from the cervix using a small brush or spatula. The cells are then sent to a lab to be examined under a microscope for any abnormalities. Pap tests can detect abnormal cells in the cervix before they become cancerous, which can help prevent cervical cancer or catch it at an early stage when it is highly treatable.
- HPV test: An HPV test looks for the presence of HPV in the cells of the cervix. This test may be done in conjunction with a Pap test in women over the age of 30, or as a follow-up to an abnormal Pap test. HPV testing can help identify women who are at increased risk of developing cervical cancer and may need more frequent screening or further testing.
It is important for women to follow the recommended screening guidelines for cervical cancer, which may vary depending on factors such as age, sexual history, and other risk factors. Women who have any symptoms of cervical cancer, such as abnormal vaginal bleeding, unusual discharge, or pelvic pain, should also see their healthcare provider for evaluation. Early detection and treatment are key to improving outcomes for women with cervical cancer.
Pap Test Result
A Pap test result can be either normal or abnormal. If the results are normal, it means that no abnormal cells were found in the sample collected from the cervix. This is good news, but it is important to remember that a normal Pap test does not completely rule out the possibility of cervical cancer or other gynecological problems.
If the results are abnormal, it means that some of the cells collected during the Pap test looked different from normal cells under the microscope. Abnormal Pap test results do not necessarily mean that a woman has cervical cancer, but they may indicate the presence of precancerous or cancerous cells. Further testing or treatment may be necessary, depending on the specific type and severity of the abnormality.
It is important for women to discuss their Pap test results with their healthcare provider and follow any recommended follow-up testing or treatment. Regular Pap tests and follow-up care are key to preventing and detecting cervical cancer at an early stage when it is highly treatable.
HPV Test Result
The HPV test result can be positive or negative.
- A negative result means that you don’t have the type of HPV that can cause cervical cancer, and your doctor may recommend waiting for your next screening test for up to five years.
- A positive result means that you have an HPV type that may be linked to cervical cancer, but it doesn’t mean you have cancer now. Your doctor may recommend further testing to identify the specific HPV type and determine the next steps.
When to Get Screened
The American Cancer Society (ACS) recommends the following guidelines for cervical cancer screening:
- Women should start getting regular Pap tests at age 21.
- Between ages 21 and 29, women should have a Pap test every three years.
- Between ages 30 and 65, women should have a Pap test and HPV test every five years. Alternatively, they may continue to have a Pap test alone every three years.
- Women over age 65 who have had regular screenings with normal results should not be screened for cervical cancer unless they have a history of cervical pre-cancer or cancer, or a weak immune system.
- Women who have had a total hysterectomy (removal of the uterus and cervix) for non-cancerous reasons do not need to be screened for cervical cancer.
However, it is important for women to discuss their individual risk factors and screening recommendations with their healthcare provider, as some women may need more frequent or earlier screening, and some may be able to stop screening after a certain age or if they have had a hysterectomy.
Stages of Cervical Cancer
Cervical cancer is typically staged using the FIGO (International Federation of Gynecology and Obstetrics) system, which takes into account the size of the tumor, how deeply it has invaded nearby tissues, and whether it has spread to lymph nodes or distant parts of the body. The stages of cervical cancer are as follows:
- Stage 0: This stage, also known as carcinoma in situ, refers to abnormal cells that are found only on the surface of the cervix and have not invaded deeper tissues.
- Stage I: The cancer is confined to the cervix and has not spread to other parts of the body. Stage I is divided into two sub-stages:
- Stage IA: The cancer is small and confined to the cervix.
- Stage IB: The cancer has grown larger, but is still confined to the cervix.
- Stage II: The cancer has spread beyond the cervix and into nearby tissues, such as the upper part of the vagina or the tissue around the uterus. Stage II is also divided into two sub-stages:
- Stage IIA: The cancer has invaded nearby tissues, but not to the pelvic wall.
- Stage IIB: The cancer has spread to the pelvic wall.
- Stage III: The cancer has spread to the lower part of the vagina or to the walls of the pelvis, and may be blocking the ureters (the tubes that carry urine from the kidneys to the bladder). Stage III is also divided into two sub-stages:
- Stage IIIA: The cancer has spread to the lower third of the vagina, but not to the pelvic wall.
- Stage IIIB: The cancer has spread to the pelvic wall or is blocking the ureters.
- Stage IV: The cancer has spread to distant parts of the body, such as the lungs, liver, or bones.
The specific stage of cervical cancer is important in determining the most appropriate treatment options and the likelihood of a cure or long-term survival.
Treatment of Cervical Cancer
The treatment of cervical cancer depends on several factors, including the stage of the cancer, the size and location of the tumor, and the woman’s overall health and personal preferences. Treatment options for cervical cancer may include one or a combination of the following:
- Surgery: Surgery may be recommended for early-stage cervical cancer to remove the cancerous tissue. In some cases, a hysterectomy (removal of the uterus) may be necessary. Lymph nodes may also be removed during surgery to determine if the cancer has spread.
- Radiation therapy: Radiation therapy may be used alone or in combination with surgery for treating cervical cancer. It uses high-energy X-rays or other types of radiation to kill cancer cells.
- Chemotherapy: Chemotherapy is a medication-based treatment that uses drugs to kill cancer cells. It may be used in combination with radiation therapy or surgery for cervical cancer treatment.
- Targeted therapy: This treatment is aimed at specific proteins or genes in the cancer cells to stop the growth and spread of cancer cells.
- Palliative care: Palliative care is used to relieve the symptoms and improve the quality of life of women with advanced cervical cancer. This type of care is provided by a team of healthcare professionals, including doctors, nurses, and social workers.
The choice of treatment and the specific approach depend on various factors such as the stage of the cancer, the patient’s general health, the patient’s preferences, and the availability of resources. Treatment is often most effective when cervical cancer is detected and treated in its early stages. Therefore, regular screening tests are important for women to detect the cancer at an early stage when it is most treatable.
NYGS Approach
At New York Gynecology Surgery (NYGS), we have a team of expert oncologists who will guide you through your cancer diagnosis and answer any questions you have. We are dedicated to meeting your specific needs and exceeding your expectations. If you or a loved one is experiencing symptoms of cancer, please call us as soon as possible.
Pankaj Singhal, MD, MS, MHCM
- Industry expertise with over 12 years of experience in both academic & private health care settings, physician practice management and executive leadership.
- Trained over 45 gynecologic surgeons along with training fellows in minimally invasive gynecologic surgery and gynecology oncology, and has developed cutting edge, new surgical techniques for endometriosis and laparoscopic surgeries.
- One of the very few surgeons who have completed over 5,718 robot-assisted gynecologic surgeries in the entire United States.
- Known for taking on the most challenging surgery cases that other doctors/centers turn away.

Hear From Our Clients

Joetta Simonette
On May 3, 2018 at Good Samarital Hospital, due to cancer, you performed ovarian surgery on me.
It is now 5 years since that date – 5 years of wellness that has been accomplished through the grace of God guiding your hands and the support of your team and my loving family.
You are an excellent, compassionate and caring doctor who was confident of a good outcome, and so it is!
Thank you, thank you for these past wonderful years. May God continue to bless you. You are in my prayers!

RG Petkos
Power couple Dr. Singhal & Dr. Mclean are amazing!! My experience with them has been absolutely wonderful. I highly recommend either of them for so many reasons mainly for helping me get back some quality of life with my successful full hysterectomy being better than I expected.
The process from the beginning with them was a pleasure and I had quite a challenge beforehand so I’m very grateful that quality, professional, caring doctors still exist!!
I especially appreciate their proactive approach and feel the combination of the care and expertise they provide make for successful outcomes!!

Kimberly Quinde
Dr. Singhal was the doctor who took care of my mother Ivonne Guevara. My mother had gone to 2 other doctors who refused to take care of her fibroid. She was in pain for years and her fibroid had grown really big without her knowing. When my mom went to Dr Singhal she was met with calmness and reassurance that everything will be ok and he would help her get better. Dr. Singhal was so kind and caring all throughout the process.
He took all her worries away and my mom highly recommends him. She hopes every doctor can be as great as Dr. Singhal.
Everyone in his office was so nice to my mom and it was a great experience given the circumstances.