Uterine Cancer
What is Uterine Cancer?
Cancer is a disease characterized by uncontrolled cell growth in the body. Typically, cancer is named based on the part of the body where it originates, even if it spreads to other parts later.
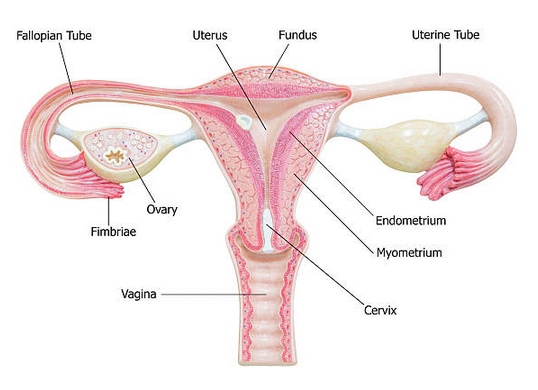
Uterine cancer, also known as endometrial cancer, occurs when cancer cells start growing in the uterus. The uterus is a pear-shaped organ located in a woman’s pelvis between the hip bones, where a developing fetus grows during pregnancy.
Endometrial cancer is the most common type of uterine cancer, as it develops in the lining of the uterus known as the endometrium. Although all women with a uterus are at risk for uterine cancer, the risk tends to increase with age, and most cases are diagnosed in women who have already gone through or are going through menopause, which marks the end of menstruation.
The American Cancer Society (ACS) predicts that approximately 65,950 new cases of uterine cancer will be detected in the United States in 2022, with postmenopausal women being the most commonly affected. The average age at which this cancer is usually diagnosed is 60.
Types of Uterine Cancer
Uterine cancer has two primary types that develop in different parts of the uterus:
- Endometrial cancer: This is the most common type of uterine cancer, accounting for more than 90% of cases. It starts in the cells of the endometrium, which is the lining of the uterus.
- Uterine sarcoma: This is a less common type of uterine cancer that starts in the muscle or other tissues of the uterus. It accounts for less than 10% of uterine cancers.
Symptoms of Uterine Cancer
Abnormal vaginal discharge or bleeding that is unusual for you may be a symptom of uterine cancer. Bleeding may be considered abnormal if it occurs after menopause or between periods, or if it is heavier than usual. It’s important to note that bleeding after periods have stopped is never considered normal. Uterine cancer may also cause pelvic pain or pressure.
If you experience abnormal bleeding, particularly if you have already gone through menopause, it’s crucial to see a doctor immediately. Additionally, if you have any other signs or symptoms that persist for two weeks or more, it’s important to seek medical attention. While these symptoms could be due to other conditions, the only way to determine the cause is to consult with your doctor.
Causes of Uterine Cancer
Uterine cancer occurs when cells in the uterus grow and multiply abnormally, leading to the formation of a tumor. The exact cause of uterine cancer is unknown, but certain factors have been identified that increase a woman’s risk of developing this disease. These risk factors include:
- Age: The risk of uterine cancer increases as women get older, especially after menopause.
- Hormonal imbalances: An excess of estrogen or a lack of progesterone in the body can increase the risk of uterine cancer.
- Obesity: Being overweight or obese increases the risk of uterine cancer.
- Diabetes: Women with diabetes have a higher risk of developing uterine cancer.
- Family history: Women who have a family history of uterine, ovarian, or colorectal cancer have a higher risk of developing uterine cancer.
- Endometrial hyperplasia: This is a condition where the lining of the uterus grows too thick, which can increase the risk of developing uterine cancer.
- Tamoxifen: This medication, which is used to treat breast cancer, can increase the risk of uterine cancer.
Lower Your Chance of Getting Uterine Cancer
There are no known methods to completely prevent uterine cancer. However, some factors may lower your risk of developing uterine cancer:
- Using birth control pills.
- Maintaining a healthy weight and being physically active.
- Taking progesterone along with estrogen.
It is advisable to consult your doctor regarding how often you should undergo screening for uterine cancer, particularly if you believe that you have risk factors that increase your chances of getting it. While these measures may aid in reducing the risk of uterine cancer, they are not recommended for everyone and have associated risks and benefits. For instance, birth control pills may increase the risk of breast cancer.
Detection of Uterine Cancer
Uterine cancer can be detected through various tests and procedures. The doctor may perform a pelvic exam to check for any abnormality or growths in the uterus. Imaging tests such as transvaginal ultrasound, CT scan, and MRI can also help detect any abnormal growth or mass in the uterus.
- A biopsy is the most reliable way to diagnose uterine cancer. It involves removing a small piece of tissue from the uterus for examination under a microscope. There are different types of biopsies, including endometrial biopsy, dilation and curettage (D&C), and hysteroscopy.
- An endometrial biopsy is performed in the doctor’s office by inserting a thin, flexible tube through the cervix into the uterus to collect a sample of the endometrial tissue. D&C involves dilating the cervix and scraping the lining of the uterus to collect a tissue sample. Hysteroscopy involves using a thin, lighted tube with a camera to view the inside of the uterus and remove a tissue sample.
- If uterine cancer is diagnosed, additional tests such as a chest X-ray, CT scan, or MRI may be performed to determine the stage and extent of the cancer.
Stages of Uterine Cancer
The process of determining the location and extent of cancer in the body, as well as whether it has spread and is affecting other parts of the body, is referred to as staging. Diagnostic tests are used by doctors to determine the cancer’s stage, and information based on tissue samples collected during surgery may be required.
Because of this, staging may not be complete until all tests are finished and the tumor has been removed through surgery (see Types of Treatment). Knowing the stage is important as it helps the doctor suggest the most effective treatment and can also assist in predicting the prognosis, or the likelihood of recovery. Different stage descriptions are used for different types of cancer. The staging system used for uterine cancer is the one developed by the International Federation of Obstetrics and Gynecology (FIGO).
The stage provides a common way of describing the cancer, enabling doctors to work together to plan the best treatments. Doctors assign the stage of endometrial cancer using the FIGO system.
Stage I: The cancer is found only in the uterus or womb, and it has not spread to other parts of the body.
- Stage IA: The cancer is found only in the endometrium or less than one-half of the myometrium.
- Stage IB: The tumor has spread to one-half or more of the myometrium.
Stage II: The tumor has spread from the uterus to the cervical stroma but not to other parts of the body.
Stage III: The cancer has spread beyond the uterus, but it is still only in the pelvic area.
- Stage IIIA: The cancer has spread to the serosa of the uterus and/or the tissue of the fallopian tubes and ovaries but not to other parts of the body.
- Stage IIIB: The tumor has spread to the vagina or to the tissue immediately next to the uterus called the parametrium.
- Stage IIIC1: The cancer has spread to the regional pelvic lymph nodes. Lymph nodes are small, bean-shaped organs that help fight infection.
- Stage IIIC2: The cancer has spread to the para-aortic lymph nodes with or without spread to the regional pelvic lymph nodes.
Stage IV: The cancer has metastasized to the rectum, bladder, and/or distant organs.
- Stage IVA: The cancer has spread to the mucosa of the rectum or bladder.
- Stage IVB: The cancer has spread to lymph nodes in the groin area, and/or it has spread to distant organs, such as the bones or lungs.
Grade
The medical professionals also classify this form of cancer by its grade (G), which reflects the degree of similarity between cancer cells and healthy cells under a microscope. By examining the cancerous tissue alongside healthy tissue, doctors can determine if the cancer cells have similar cell groupings to healthy cells, which is known as “differentiated” or “low-grade tumor,” or if the cancer cells look significantly different from healthy tissue, which is referred to as “poorly differentiated” or “high-grade tumor.” The grade of cancer may help doctors forecast how rapidly the cancer will develop. In general, a slower growth rate is associated with a more favorable prognosis.
The letter “G” is used to define a grade for uterine cancer.
- GX: The grade cannot be evaluated.
- G1: The cells are well differentiated.
- G2: The cells are moderately differentiated.
- G3: The cells are poorly differentiated.
Treatment of Uterine Cancer
In case you have been diagnosed with uterine cancer, you can request your doctor to refer you to a gynecologic oncologist, a specialist who is trained to treat such cancers. You can work together with this doctor and their team to develop a treatment plan.
Types of Treatment
There are several treatment options for uterine cancer, including:
- Surgery: The most common treatment for uterine cancer is surgery to remove the uterus (hysterectomy). The surgeon may also remove the fallopian tubes, ovaries, and nearby lymph nodes. In some cases, a woman may be able to have a minimally invasive surgery instead of an open surgery.
- Radiation therapy: Radiation therapy uses high-energy radiation to kill cancer cells. It can be given externally (from outside the body) or internally (from inside the body).
- Chemotherapy: Chemotherapy is a drug treatment that kills cancer cells. It may be given before surgery to shrink the tumor or after surgery to kill any remaining cancer cells.
- Hormone therapy: Hormone therapy uses drugs to block hormones that may be fueling the growth of cancer cells. This treatment is only used for certain types of uterine cancer.
The choice of treatment depends on the stage of the cancer, the grade of the cancer, the woman’s age and overall health, and other factors. The treatment plan is usually developed by a team of doctors, including a gynecologic oncologist, who specializes in treating cancers of the female reproductive system.
NYGS Approach
We understand that a cancer diagnosis can be overwhelming and scary. Here at New York Gynecology Surgery (NYGS), we build our teams around you. Our expert oncologists will help guide you through this difficult time, answering any questions you may have along the way. We are here for you and will do everything in our power to meet your specific needs and exceed your expectations.
If you or a loved one is experiencing symptoms that may be related to cancer, please call us as soon as possible.
Pankaj Singhal, MD, MS, MHCM
- Industry expertise with over 12 years of experience in both academic & private health care settings, physician practice management and executive leadership.
- Trained over 45 gynecologic surgeons along with training fellows in minimally invasive gynecologic surgery and gynecology oncology, and has developed cutting edge, new surgical techniques for endometriosis and laparoscopic surgeries.
- One of the very few surgeons who have completed over 5,718 robot-assisted gynecologic surgeries in the entire United States.
- Known for taking on the most challenging surgery cases that other doctors/centers turn away.

Hear From Our Clients

Joetta Simonette
On May 3, 2018 at Good Samarital Hospital, due to cancer, you performed ovarian surgery on me.
It is now 5 years since that date – 5 years of wellness that has been accomplished through the grace of God guiding your hands and the support of your team and my loving family.
You are an excellent, compassionate and caring doctor who was confident of a good outcome, and so it is!
Thank you, thank you for these past wonderful years. May God continue to bless you. You are in my prayers!

RG Petkos
Power couple Dr. Singhal & Dr. Mclean are amazing!! My experience with them has been absolutely wonderful. I highly recommend either of them for so many reasons mainly for helping me get back some quality of life with my successful full hysterectomy being better than I expected.
The process from the beginning with them was a pleasure and I had quite a challenge beforehand so I’m very grateful that quality, professional, caring doctors still exist!!
I especially appreciate their proactive approach and feel the combination of the care and expertise they provide make for successful outcomes!!

Kimberly Quinde
Dr. Singhal was the doctor who took care of my mother Ivonne Guevara. My mother had gone to 2 other doctors who refused to take care of her fibroid. She was in pain for years and her fibroid had grown really big without her knowing. When my mom went to Dr Singhal she was met with calmness and reassurance that everything will be ok and he would help her get better. Dr. Singhal was so kind and caring all throughout the process.
He took all her worries away and my mom highly recommends him. She hopes every doctor can be as great as Dr. Singhal.
Everyone in his office was so nice to my mom and it was a great experience given the circumstances.
Hospital Affiliations


Request an Appointment
"*" indicates required fields