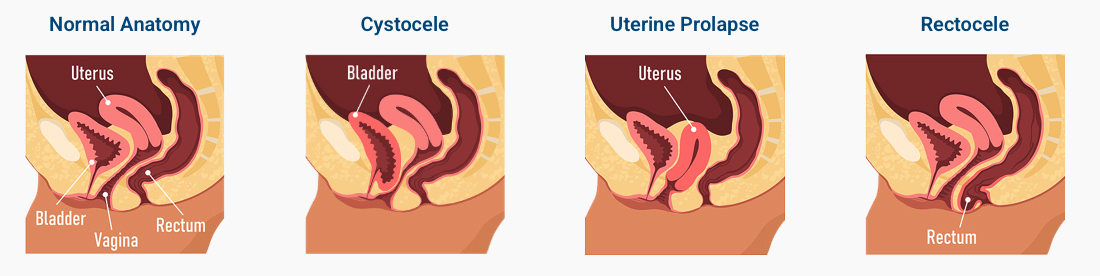
Restoring Strength, Comfort, and Confidence
Our team understands that pelvic organ prolapse can impact both physical comfort and emotional well-being. We approach every case with precision and compassion — beginning with a thorough evaluation and personalized treatment plan. Whether through pelvic floor therapy, non-surgical support devices, or advanced laparoscopic and robotic repair procedures, our goal is to restore your body’s natural balance and help you regain confidence in your daily life.