Understanding Fallopian Tube Cancer
Fallopian tube cancer is a rare but serious condition that originates in the narrow passage connecting the ovaries and uterus. Because its early symptoms often resemble other gynecologic conditions, it can be difficult to detect in its earliest stages. At New York Gynecology Surgery & Endometriosis (NYGSE), our specialists use advanced imaging, genetic insight, and minimally invasive surgical techniques to identify and treat fallopian tube cancers with precision. We’re committed to helping women receive an accurate diagnosis and the most effective, personalized treatment plan possible.
COMMON QUESTIONS ABOUT FALLOPIAN TUBE CANCER
Fallopian tube cancer, also referred to as tubal cancer, emerges within the fallopian tubes, which serve as the connecting pathway between the ovaries and the uterus. This type of cancer is exceptionally uncommon, accounting for only 1 to 2 percent of all gynecologic cancers. Globally, there have been reports of 1,500 to 2,000 cases of fallopian tube cancer. In the United States, approximately 300 to 400 women are diagnosed with this condition each year.
Interestingly, cancer more frequently originates from other parts of the body, like the ovaries or endometrium, and then spreads to the fallopian tubes rather than having its primary origin in the fallopian tubes themselves.
The typical age range of women affected by fallopian tube cancer is between 50 and 60, although it can develop at any age. Caucasians, particularly those who have had few or no children, are more prone to this type of cancer.
Due to its rarity, limited knowledge exists regarding the specific causes of fallopian tube cancer. However, researchers are exploring the potential role of genetics in its development. Some evidence suggests that women who have inherited the BRCA1 gene, which is associated with breast and ovarian cancer, may have an increased risk of developing fallopian tube cancer.
Recent findings have led doctors to consider that many high-grade serous type epithelial ovarian cancers, which are among the most common ovarian cancers, might actually initiate in the distal end of the fallopian tube, rather than on the surface of the ovary.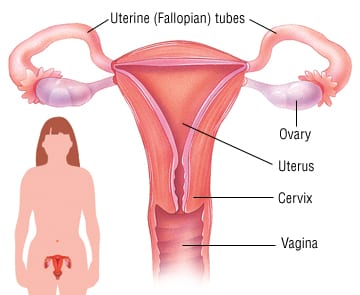
Fallopian tube cancers mainly consist of epithelial or surface carcinomas, which implies that they originate from the tissue lining or covering the fallopian tubes.
There are various types of fallopian tube cancers, including:
- Papillary serous adenocarcinomas: This type accounts for more than 95 percent of all fallopian tube cancers. It arises from the cells that line the fallopian tubes. As these cells undergo abnormal division and invade other organs or spread to different parts of the body, tumors can develop.
- Primary fallopian tube cancer: Primary fallopian tube cancer is an exceptionally rare form, making up about 1 percent of all gynecologic cancers.
- Sarcomas (leiomyosarcomas): In some cases, tumors called sarcomas (leiomyosarcomas) may originate from the smooth muscle within the fallopian tubes.
- Transitional cell carcinomas: Tumors can also form on the other cells that line the fallopian tubes, known as transitional cell carcinomas.
Detecting fallopian tube cancer can be challenging as its symptoms often overlap with those of various common conditions experienced during menopause, which is a time when this type of cancer commonly occurs.
Symptoms may include:
- Abdominal swelling
- Abdominal and back pain
- Loss of appetite or feeling full quickly
- Frequent or urgent need to urinate, along with changes in toilet patterns, such as alterations in bowel habits
- Unexplained weight loss or gain
- Indigestion or heartburn
- Fatigue
- Watery discharge from the vagina.
If you experience any of these symptoms, it’s essential to consult your doctor. While these signs could be attributed to causes other than cancer, seeking medical advice is the only way to determine the underlying cause accurately.
The specific cause of fallopian tube cancer remains unknown; however, certain factors are suspected to increase the risk, including: cost like 600
- Advancing age (most cases are diagnosed in women between 50 and 60 years old).
- Post-menopausal status.
- Nulliparity (having no children).
- Family history of ovarian or breast cancer, particularly among close relatives (mother, sister, daughter).
- Increased risk associated with inherited mutations in the BRCA gene, which are linked to higher incidences of ovarian and breast cancers.
- Never having breastfed a child.
- Never having used birth control pills.
- Presence of endometriosis, a benign (non-cancerous) condition that can elevate the risk of ovarian and fallopian tube cancers.
Various factors contribute to different types of cancer, and researchers are actively investigating the causes and prevention of ovarian and fallopian tube cancer. While there is no definitive way to completely prevent these cancers, it may be possible to lower one’s risk. Consulting your healthcare team can provide valuable insights into your individual cancer risk.
Studies have indicated that certain factors may reduce the risk of developing ovarian and fallopian tube cancer:
- Taking birth control pills: Individuals who have used oral contraceptives for three or more years have shown a 30% to 50% lower likelihood of developing ovarian and fallopian tube cancer. This decreased risk might persist for up to 30 years after discontinuing the pills. Additionally, intrauterine devices (IUDs) have been associated with a reduced risk of ovarian cancer.
- Breastfeeding: Prolonged breastfeeding after childbirth is linked to a decreased risk of ovarian and fallopian tube cancer.
- Pregnancy: The number of full-term pregnancies a person has experienced is inversely related to their risk of ovarian and fallopian tube cancer.
- Surgical procedures: People who have undergone a hysterectomy or tubal ligation tend to have a lower risk of developing ovarian and fallopian tube cancer. A hysterectomy involves removing the uterus and sometimes the cervix. Tubal ligation is a surgical procedure where the fallopian tubes are tied or closed to prevent pregnancy. For individuals at high risk of ovarian and fallopian tube cancer, doctors might recommend bilateral salpingo-oophorectomy, which involves removing both ovaries and fallopian tubes. Some individuals choose to have their fallopian tubes removed during abdominal surgery for other purposes or during a caesarean section after completing their desired number of childbirths.
- High-risk genetic mutations: Individuals with genetic mutations like BRCA1, BRCA2, and genes associated with Lynch syndrome are advised to consider removing their ovaries and fallopian tubes after completing childbearing. This preventive measure can reduce the risk of ovarian and fallopian tube cancers by up to 96%. Furthermore, if the surgery is performed before natural menopause, there may be a 40% to 70% decrease in the risk of developing breast cancer, especially for individuals with BRCA2 mutations.
Due to the rarity of fallopian tube cancer and its symptoms resembling other conditions, diagnosing it can be challenging. Sometimes, women only discover they have fallopian tube cancer when a tube is surgically removed during treatment for another health issue.
However, several tests can aid in definitively diagnosing the condition. Your doctor will begin by inquiring about any symptoms you may be experiencing, reviewing your medical history, and conducting a thorough physical examination. Additional tests that may be performed include:
- Pelvic Exam: This involves the examination of the uterus, vagina, ovaries, fallopian tubes, bladder, and rectum to detect any abnormalities in size or shape.
- CA125 Test: A blood test to measure CA125 levels, a tumor marker associated with gynecological diseases, including fallopian tube cancer. While approximately 85 percent of women with gynecological diseases have elevated CA125 levels, it’s crucial to note that increased CA125 levels may not necessarily indicate cancer. Levels can also rise during pregnancy, menstruation, and other non-cancerous gynecological diseases or cancers affecting different parts of the body.
- Computed Tomography (CT) Scan: This imaging test captures detailed pictures of the body’s internal areas. A computer, linked to an X-ray machine, generates these images. To enhance organ or tissue visibility, a special dye may be injected into a vein or swallowed.
- Ultrasound: Pelvic ultrasound uses high-frequency sound waves to create images of organs and systems within the body. These sound waves, inaudible to humans, produce a pattern of echoes called a sonogram, which can differentiate between healthy tissues, fluid-filled cysts, and tumors.
- PET (Positron Emission Tomography): PET scans involve the use of a radioactive sugar (glucose) to identify cancer cells. This test is sometimes employed to detect the spread of fallopian tube cancer.
These tests collectively aid in achieving an accurate diagnosis and better understanding the extent of fallopian tube cancer if present.
The stages of fallopian tube cancer are determined by the extent of its spread, ranging from the earliest (Stage I) to the most advanced (Stage IV):
- Stage I: Cancer is confined to one or both fallopian tubes.
- Stage II: Cancer has extended to the uterus or nearby tissues within the pelvic region (which includes internal reproductive organs, bladder, and rectum), or it is localized on the peritoneum.
- Stage III: Cancer has progressed beyond the pelvic region and spread to lymph nodes and/or other abdominal areas (such as the surface of the liver or spleen).
- Stage IV: Cancer has metastasized to distant locations, such as the lungs.
Surgery plays a crucial role in the treatment of ovarian and fallopian tube cancers, and it is typically carried out by a gynecologic oncologist, a specialist in treating gynecologic cancers, including surgical procedures and chemotherapy (see “Chemotherapy” below).
As mentioned earlier in the Diagnosis section, surgery is often necessary to fully assess the extent of the disease and establish an accurate stage. Minimally invasive surgery is commonly employed to confirm the diagnosis and determine whether a debulking procedure (see below) should be performed immediately after diagnosis or after administering chemotherapy first. This step is essential because imaging tests may not always reveal the complete extent of the disease.
For patients with localized cancer in the ovary, a debulking procedure includes a staging process, involving the removal of various tissues, including lymph nodes, to determine if the cancer has spread. In advanced cases, the primary objective is to remove as much cancer as possible. This procedure has been shown to be most effective when combined with chemotherapy after the surgery.
There are several surgical options for ovarian and fallopian tube cancer, and the recommended surgeries depend on the tumor’s stage. In some cases, multiple procedures may be performed during the same surgery:
- Salpingo-oophorectomy: This surgery involves the removal of the ovaries and fallopian tubes. When both ovaries and both fallopian tubes are removed, it is referred to as bilateral salpingo-oophorectomy. For individuals with early-stage cancer who desire future pregnancy, it may be possible to remove only one ovary and one fallopian tube if the cancer is limited to one ovary. This type of surgery is known as unilateral salpingo-oophorectomy. For patients with a germ cell type of ovarian tumor, it is often sufficient to remove only the ovary containing the tumor, preserving the ability to conceive.
- Hysterectomy: This procedure involves the removal of the uterus and surrounding tissue if necessary. If only the uterus is removed, it is called a partial hysterectomy. A total hysterectomy includes the removal of both the uterus and the cervix.
- Lymphadenectomy/lymph node dissection: During this surgery, the surgeon may remove lymph nodes in the pelvic and paraortic regions.
- Omentectomy: This surgery aims to remove the thin tissue covering the stomach and intestines.
- Cytoreductive/debulking surgery: Used for advanced ovarian and fallopian tube cancers, the goal of this surgery is to remove as much tumor as safely possible. It may involve removing tissue from nearby organs, such as the spleen, liver, and parts of the small bowel or colon. This can alleviate symptoms caused by masses pressing on other organs and enhance the effectiveness of subsequent treatments, such as chemotherapy, to control any remaining disease. If the cancer has spread beyond the ovaries, fallopian tubes, or peritoneum, doctors may use neoadjuvant chemotherapy to shrink the tumor before cytoreductive or debulking surgery. Neoadjuvant chemotherapy involves 2 to 3 cycles of chemotherapy before the surgery to make the debulking procedure safer and more effective. Hyperthermic intraperitoneal chemotherapy (HIPEC), a newly described method, is being studied in clinical trials and is not yet the standard of care. Sometimes, chemotherapy may be administered during surgery.
It is advisable to have debulking surgery performed by a board-certified gynecologic oncologist if possible. Before undergoing surgery, discuss the risks and benefits of the procedure with your doctor. Inquire about the surgeon’s experience with debulking surgery and whether it will be conducted minimally invasively, through an open incision, or robotically. Make sure to explore the various surgical options with your doctor.
The treatment plan may involve medications aimed at destroying cancer cells. These medications can be administered through the bloodstream to target cancer cells throughout the body, a process known as systemic therapy. Alternatively, medication may be applied directly to the cancer or confined to a specific area of the body, which is referred to as local therapy.
A medical oncologist, a specialist in cancer treatment with medication, typically prescribes this form of treatment. Medications are often administered through an intravenous (IV) tube inserted into a vein using a needle or in the form of oral pills or capsules that are swallowed. When given intravenously, a port, a small plastic or metal disc placed under the skin before treatment begins, is often used to access the vein. For patients receiving oral medications, it’s essential to inquire about proper storage and handling guidelines from the healthcare team.
The types of medications used for ovarian, fallopian tube, and peritoneal cancer include:
- Chemotherapy
- Targeted therapy
- Immunotherapy
- Hormone therapy (in rare cases)
An individual may receive a single type of medication or a combination of medications simultaneously to treat their cancer. These medications may also be included as part of a comprehensive treatment plan that involves surgery and/or radiation therapy.
The medications used for cancer treatment are continually under evaluation. Discussing these medications with your doctor is crucial to understanding their purpose, potential side effects, and possible interactions with other medications. It’s essential to inform your doctor about any other prescriptions, over-the-counter medications, or supplements you may be taking. Certain herbs, supplements, and other drugs can interact with cancer medications, leading to unwanted side effects or reduced effectiveness. Utilizing searchable drug databases can help you gain more information about your prescriptions.
Radiation therapy is not a primary treatment for ovarian or fallopian tube cancer. It may be used in select situations—such as early-stage clear cell ovarian cancer after chemotherapy, or for small, localized recurrences. It can also help manage symptoms or treat cancer that has spread.
Radiation therapy uses high-energy x-rays or particles to destroy cancer cells. Most patients receive external-beam radiation, delivered by a machine outside the body. Less commonly, internal radiation (brachytherapy) is used, in which a small radioactive source is placed near the tumor.
Proton therapy, a newer form of treatment, targets tumors more precisely by using protons instead of x-rays.
Typical side effects include fatigue, mild skin irritation, stomach upset, and loose stools, which usually resolve soon after treatment.
Radiation may also be part of care for recurrent or metastatic disease, often in combination with chemotherapy, targeted therapy, or immunotherapy to improve control and comfort. In advanced cases, palliative radiation can help relieve pain or other symptoms.
Because every case is unique, your treatment plan should be developed by a gynecologic oncologist in consultation with radiation and medical oncologists experienced in ovarian and fallopian tube cancers.
We understand that a cancer diagnosis can be overwhelming and scary. Here at NYGSE, we build our teams around you. Our expert oncologists will help guide you through this difficult time, answering any questions you may have along the way. We are here for you and will do everything in our power to meet your specific needs and exceed your expectations.
If you or a loved one is experiencing symptoms that may be related to cancer, please call us as soon as possible.
Types of Gynecologic Cancer

Pankaj Singhal, MD, MS, MHCM
With over 12 years of experience in both academic and private healthcare, Dr. Singhal has trained more than 45 gynecologic surgeons and fellows in minimally invasive and oncologic procedures. He has pioneered new surgical techniques for endometriosis and laparoscopic surgery, completing more than 5,700 robotic-assisted cases nationwide. Renowned for taking on the most complex cases other centers turn away, Dr. Singhal continues to advance the standard of women’s surgical care.