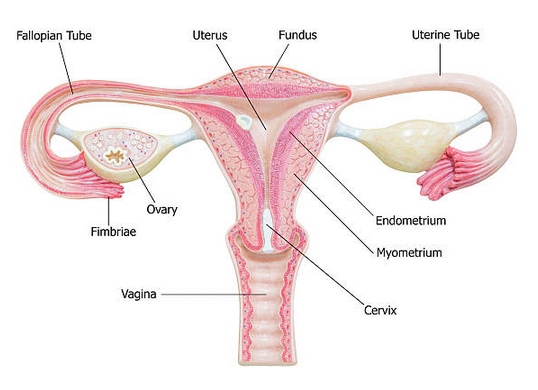
Opportunistic salpingectomy is a surgical procedure involving the removal of the fallopian tubes. This surgical intervention is typically performed in conjunction with other planned pelvic surgeries and is often recommended for individuals who have completed their family planning and wish to reduce their risk of developing certain types of cancer.
The removal of the fallopian tubes during opportunistic salpingectomy has been shown to lower the risk of epithelial ovarian cancer, fallopian tube cancer, and peritoneal cancer. This preventive measure is especially beneficial for individuals who are at a higher risk for these types of cancer due to genetic factors or other risk factors. By removing the fallopian tubes, which can be a site of cancer development, opportunistic salpingectomy offers a proactive approach to cancer risk reduction, providing individuals with peace of mind and a potential safeguard against these life-threatening diseases.
Importance of Opportunistic Salpingectomy in Ovarian Cancer
Studies indicate that the predominant and deadliest forms of ovarian cancer originate within the fallopian tubes. Since ovarian cancer lacks effective screening methods and symptoms typically manifest at advanced stages, this procedure offers a potent risk-reduction strategy for individuals with an average risk profile.
Opportunistic salpingectomy plays a significant role in reducing the risk of ovarian cancer, and its importance in ovarian cancer prevention cannot be overstated. Here are several key reasons why opportunistic salpingectomy is important in the context of ovarian cancer:
- Effective Cancer Risk Reduction: Ovarian cancer is often diagnosed at an advanced stage, making it challenging to treat effectively. By removing the fallopian tubes during opportunistic salpingectomy, which are a common site of origin for certain types of ovarian cancer, the risk of developing this deadly disease is significantly reduced. This proactive measure can be particularly crucial for individuals at a higher risk of ovarian cancer, such as those with a family history of the disease or certain genetic mutations (e.g., BRCA1 and BRCA2).
- Minimally Invasive: Opportunistic salpingectomy can be performed during other planned pelvic surgeries, such as hysterectomies or tubal ligations. This minimizes the need for additional surgeries and recovery time. It’s a relatively straightforward procedure that can be seamlessly integrated into other gynecological interventions.
- No Impact on Hormones or Menopause: Unlike some other preventive measures like oophorectomy (removal of ovaries), which can induce early menopause and hormonal imbalances, opportunistic salpingectomy does not interfere with hormonal function. This means individuals can maintain their hormonal balance and overall quality of life.
- Reproductive Choice: Opportunistic salpingectomy is a suitable option for individuals who have completed their family planning and do not wish to have more children. It can be a part of a comprehensive family planning strategy, offering both cancer prevention and contraception simultaneously.
- Long-Term Benefits: The protective effect of opportunistic salpingectomy lasts beyond the surgery itself. By reducing the risk of ovarian cancer, individuals can potentially enjoy a longer and healthier life, free from the physical and emotional burdens associated with ovarian cancer treatment.
Who Should Consider Opportunistic Salpingectomy?
Opportunistic salpingectomy is a valuable consideration for individuals at average risk of ovarian cancer, particularly those who have completed their family planning and do not wish to have more children. This procedure offers a proactive approach to reducing the risk of ovarian cancer, a disease known for its late-stage diagnosis and high mortality rates. By removing the fallopian tubes, which have been linked to the origin of many ovarian cancers, opportunistic salpingectomy provides a minimally invasive and effective means of cancer risk reduction. It is a suitable choice for those seeking to safeguard their long-term health and well-being without impacting hormonal balance or fertility.
Additionally, opportunistic salpingectomy is especially relevant for individuals with a heightened risk of ovarian cancer due to genetic factors or a family history of the disease. Those with known genetic mutations such as BRCA1 and BRCA2, which significantly elevate ovarian cancer risk, can benefit from this preventive measure. Moreover, individuals scheduled for other pelvic surgeries, such as hysterectomies or tubal ligations, can seamlessly incorporate opportunistic salpingectomy into their procedures, optimizing their overall health management.
Key Data on Opportunistic Salpingectomy and Ovarian Cancer
- According to Herzog et al. (2013), approximately 75%–80% of ovarian cancers, especially the high-grade serous and undifferentiated types, have their origins in the fallopian tube.
- The Society of Gynecologic Oncology of Canada recommends bilateral salpingo-oophorectomy (BSO) for high-risk individuals with BRCA mutations, as it significantly reduces the risk of ovarian cancer.
- Bilateral salpingectomy can reduce the risk of ovarian cancer by 40% (Aggarwal et al, 2016).
- Opportunistic Salpingectomy with ovarian retention may be preferable for young, low-risk premenopausal women to avoid the potential health risks associated with elective BSO (Aggarwal et al, 2016).